Physical Therapy Guide to Torticollis
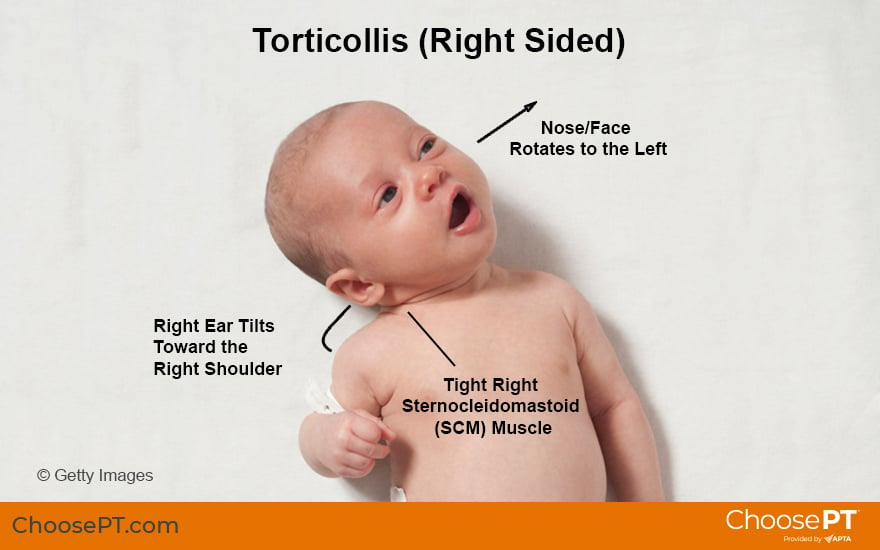
Torticollis — or simply, twisted neck — is a condition in which the head stays tilted to one side. Infant torticollis is due to a tight neck muscle. Generally, the infant tips their ear toward one shoulder while the face turns toward the opposite side. Some children are born with torticollis, but it most often develops after birth. Infant torticollis may result from the baby's position in the womb or from too much time spent lying on their back or in containers (such as car seats and swings). As many as 16% of newborns (1 in 6) experience torticollis. Having a flat head ( plagiocephaly) and torticollis often occur together. Infant torticollis responds very well to physical therapy. The earlier treatment begins, the more quickly and completely it can be resolved.
Physical therapists are movement experts who use the latest evidence to design treatment plans for each person's needs and goals. They improve quality of life through hands-on care, patient education, and prescribed movement. You can contact a physical therapist directly for an evaluation. To find a physical therapist in your area, visit Find a PT .
What Is Infant Torticollis?
Infant torticollis happens when a neck muscle (called the sternocleidomastoid, or SCM, muscle) is shortened or too tight. The SCM muscle starts behind the ear and attaches to the collarbone and breastbone. With a shortened or tight SCM, the child’s neck is bent to one side and the head is rotated to the opposite side. Torticollis can be present at birth. It also can develop later as a result of a flat skull or too much time spent in the same position (such as lying on their back or sitting in a car seat or bouncy seat).
If untreated, this condition can lead to an uneven posture of the whole body. Torticollis affects the entire child and is not just a head and neck issue.
Torticollis has three diagnosis groups:
Group 1: sternocleidomastoid "tumor" torticollis, or SCM. With this type of torticollis, there is not an actual tumor. Rather, a bulge of tissue develops in the muscle due to a lack of length in the infant’s neck. This is considered the most severe form of torticollis and may take the longest to treat. It results in neck muscle tightness and loss of neck range of motion/flexibility.
Group 2: muscular torticollis. Children with this condition have neck muscle tightness and loss of neck range of motion and flexibility, but without the neck bulge.
Group 3: positional torticollis. This is the mildest and most treatable form of infant torticollis. However, if treatment stops too early, the child may return to their positional preference. Children with this type of torticollis do not have tight neck muscles and have normal neck range of motion and flexibility. They typically have one of the following:
- Strong preference for certain positions.
- Muscle imbalance.
Causes of torticollis can be:
- Muscular. This is the most common cause and includes a tight SCM or other neck muscles.
- Neurological.* These causes are less common but can include:
- A tumor in the small space inside the skull near the brain stem and cerebellum (back of the brain).
- A tumor in the eye or on the nerve for the eye.
- Sandifer syndrome (a genetic condition causing uncontrolled muscle movements in which a baby twists and arches with their back and neck).
- Skeletal.* Boney malformations (abnormal bone growth or shape) in the skull or cervical spine (neck).
*If an exam reveals a possible neurological or skeletal cause, your child's physical therapist will team up with, and refer you to, another specialist.
Other conditions that often occur along with torticollis include:
- Brachial plexus (nerve) injury . This can occur from trauma to the neck, shoulder, or arm during a difficult delivery that damaged the nerves controlling the shoulder, arm, and hand muscles.
- Hip dysplasia. This is a condition where the ball of the thigh bone (femur) does not fit well with the hip socket (pelvis) as it should.
- Plagiocephaly or brachycephaly (a flattened or uneven head shape).
- Delayed motor skill development.
Situations that may lead to a baby being born with torticollis include:
- Longer body length. Research notes infants with a body length of 19.7 to 20.4 inches have an 88% increased risk of torticollis.
- Lack of space in the uterus for the growing baby (more common with multiple fetuses).
- Poor positioning of the fetus. Some mothers report their baby "felt stuck" during the final weeks of pregnancy. Poor positioning can lead to pressure on one area of the skull, causing:
- An uneven or flat head.
- Jaw tilt.
- Uneven facial features (face bones are not fully developed).
- Limited range of motion/flexibility.
It is important to note a baby’s parents could not have changed any of the factors listed in this section and did not cause this diagnosis.
Older children and adults can develop torticollis due to:
- Trauma.
- Inflammation or infection.
- Vision problems or imbalances.
- Neurological conditions.
- Chronic poor alignment of the head and neck.
Since the early 90s, the number of infant torticollis cases has grown dramatically. Major factors contributing to the increase include the following changes in the modern infant's environment:
- The American Academy of Pediatrics "Back to Sleep" campaign encouraged parents to place babies on their backs to sleep. The campaign, which started in 1992, lowered the rate of sudden infant death syndrome by 50%. It led to 87% of newborns sleeping on their backs, but an increase in the rate of infants with head-shape flatness and, thus, torticollis. Note: Babies should still be placed on their backs to sleep to reduce the risk of SIDS but should have ample “tummy time” while awake.
- Babies started spending less time on their tummies due to fear of SIDS (0 to 15 minutes per day). It is recommended that babies spend several periods of time on their tummy with a caregiver present several times a day for up to an hour total.
- Parents increased their use of infant containers, such as swings, bouncy chairs, and car seats when they became more portable. As a result, more babies spend longer periods on their backs or in semi-upright positions (up to 20 hours per day).
Doctors and pediatric physical therapists began noticing changes in infant motor development. They also saw increased numbers of infants with flat spots on the head. Parents often noted a flat skull even before discovering their child preferred to hold their head to one side.
These findings lead the APTA Academy of Pediatric Physical Therapy to develop their Clinical Practice Guidelines on the diagnosis and treatment of torticollis in 2013, which also includes parent and caregiver information. As additional research and treatments have updated, the guideline was revised in 2018.
Signs and Symptoms
Common signs of infant torticollis include:
- Neck muscle(s) may be shorter or tighter on one side.
- Head often tilts to one side and stays turned to the other side.
- Limited range of motion/flexibility of the head and neck.
- A flat spot behind the ear on the side the baby prefers to turn.
- The ear may be shifted forward on the flat/preferred side.
- The forehead is shifted forward on the flat/preferred side.
- Recessed eye and smaller cheek on the side of the tight muscle/non-preferred side.
- Retracted jaw on the side of the tight muscle/nonpreferred side.
- Tongue sticking out to the side away from the tight muscle/nonpreferred side.
- Small, soft lump (SCM tumor) in the neck due to the muscle thickness and texture changes.
- Preference among breast-fed and bottle-fed babies to eat on one side over the other.
- Other feeding problems:
- Problems latching onto the breast or bottle.
- Trouble transitioning to solids and textured foods.
- Tight or restricted tongue and lip tissue (tongue or lip ties) affecting sucking and swallowing.
Infants with torticollis often also display other common signs. Parents and caregivers may notice their baby has:
- Trouble bringing their hands to the middle of the body.
- Delayed visual development (trouble with following, focusing, and using both eyes together).
- Problems with planning how to move in space (motor planning).
- Trouble with fast movements (inner ear or balance problems).
- Reflux (stomach acid flows back up into the tube connecting the stomach and mouth, causing discomfort after feeding).
- Decreased awareness of the arm and hand on the side opposite of the tight muscle.
- Decreased or limited protective responses during a loss of balance to the tight side.
- Increased lateral flexion (curved posture to one side) of the body on the tight muscle side.
- Decreased visual tracking (eye movement) to the tight side.
- Decreased muscle strength on the longer muscle (nontight) side.
- Delayed rolling over both sides or a preference to roll only over on the long (nontight) side.
How Is It Diagnosed?
Often, parents notice uneven postures or head shape changes in their baby after birth. It is vital to get an evaluation by a physical therapist as soon as you notice any signs of torticollis.
According to the American Academy of Pediatrics, doctors should screen for signs of uneven posture at every well-child visit from birth through the first six months. Infants with uneven posture should be referred to a pediatric physical therapist for further evaluation and treatment.
Newborns should receive an evaluation by a pediatric physical therapist at or shortly after birth to screen for torticollis. The sooner a baby sees a physical therapist for head and neck problems, the sooner they can address them and prevent a loss, or further loss, of muscle length. Early physical therapy for torticollis is more effective and takes less time than when treatment is delayed.
Your child's physical therapist will perform a full evaluation to assess their condition and determine any factors that may contribute to it. They will gather information about your child's health history. They also may ask you questions about your pregnancy, your child's birth, and any concerns since birth. Your child's physical therapist also will conduct a physical exam.
If an uneven neck posture is present, an ultrasound of both sides of the neck may be performed and may confirm a difference in muscle thickening and muscle texture changes as a possible cause for the torticollis. This safe, low-cost tool can help verify the amount of involvement of the tight muscle and help determine how often and how long a baby should see a physical therapist for treatment. Ultrasound also helps in monitoring your baby's progress throughout treatment.
How Can a Physical Therapist Help?
Physical therapy is the recommended treatment for torticollis. Before birth, physical therapists work with expectant parents on prevention of torticollis in their newborn. After birth, they screen newborns for muscle, bone, joint, and movement problems and provide needed treatment. Physical therapists use play to engage infants in activities and hands-on therapy to improve neck posture in a gentle, fun way. They understand how a baby communicates their tolerance for treatment and adjust treatment as needed. They also work with caregivers to create an environment that promotes development. As movement and developmental experts, pediatric physical therapists have the education, expertise, and experience necessary to screen, evaluate and diagnose postural asymmetries and should do so from birth.
Early treatment for infant torticollis reduces the risk of developing related problems. Getting physical therapy early also reduces the number of visits needed and, in the SCM tumor group, may eliminate the need for surgery. Research shows children who received physical therapy treatment and follow a home exercise program (provided by a caregiver) had better results than children who only received home exercises.
Physical therapists provide treatment to restore as much normal movement, posture, and function as possible. With proper treatment, 90%-95% of children improve or achieve an acceptable neck range of motion.
Your child's physical therapy treatment plan will depend on their exam and may include:
Passive range-of-motion exercises. Your physical therapist will perform passive neck movements and stretches with your baby. They will gently move your baby's neck toward its full range of motion. They also will teach parents and caregivers how to do these exercises for their baby at home.
Active range-of-motion exercises. Your physical therapist will work with your child to get them to move their own neck and trunk actively, using play appropriate for their age and development. They may use and teach you how to use toys or other techniques to encourage your child to do these exercises regularly.
Muscle strengthening and functional activities. Your physical therapist will work with your child to help them develop muscle strength and symmetrical (even) movement in their neck. They may use therapy balls, toys, and other special equipment to safely engage your child's muscles in many positions (on their tummy, sitting) to promote even muscle development for head and neck control.
Patient and caregiver education. Physical therapists can teach expectant parents and caregivers about the risks of, and ways to prevent, infant torticollis in their newborn, including the causes and risk factors so they can avoid them when possible. They also can inform parents about identifying the signs of infant torticollis and ways to prevent secondary problems. These may include:
- The importance of seeking care early if posture imbalances are noticed.
- Proper positioning and the importance of movement and changing positions often.
- Limiting the amount of time an infant spends in car seats, bouncer seats, carriers, and other containers.
- Ensuring babies spend as much time as possible during their awake hours in positions other than on their backs (tummy time, or simply being held and encouraged to look around).
- Teaching caregivers how to perform a home exercise program to extend treatment beyond the clinic.
Myofascial release. Your child's physical therapist may apply gentle pressure or massage to your baby’s myofascial (connective) tissues to release muscular shortness and tightness. This method can help restore motion to the tightened side of your child's neck, trunk, or back.
Vision therapy for focus and tracking. Your physical therapist will work with exercises to help improve visual focus and tracking/following objects.
Balance system therapy. Your physical therapist may work with your child on inner ear and balance training. This can help improve your child's tolerance for movement and encourage them to explore their environment on all sides.
Your physical therapist will partner with other members of your health care team as needed to address any related problems.
In rare cases, your child's doctor may recommend surgery if your baby's muscle tightness persists and limits their head movement. Surgery may be considered if your baby:
- Has a sternocleidomastoid (SCM) tumor diagnosis and is not improving with therapy.
- Has more than a 15-degree difference in neck rotation between sides that does not respond to conservative treatment.
- Has an SCM contracture causing changes to the facial bones and structure on the tight side.
- Experiences muscular torticollis that persists past one year of age and other causes and conditions have been eliminated.
Can This Injury or Condition Be Prevented?
Some cases of torticollis and flat spots on the skull occur from birth and cannot be prevented but can be treated after birth. Caregiver awareness about proper positioning of newborns can help ensure babies spend enough time on their tummy during waking hours and do not spend too much time in one position on their backs, in containers, or in baby seats. This gives newborns the best environment for their head and neck to develop normally.
Getting a referral to see, or going directly to, a physical therapist immediately after noticing a baby has an uneven posture or flat head can help prevent secondary issues. Families and caregivers should seek early screening for torticollis or a flat spot on the baby's skull. The sooner a baby is evaluated, the sooner other issues can be prevented and correction of range of motion or flattening of the skull can occur. The following tips can help you ensure your baby has a healthy environment in which to grow and develop:
- Discuss any concerns with your child's doctor if you notice any signs of torticollis or a flat spot on your baby's head.
- Ask for a referral to physical therapy from your baby's pediatrician or seek physical therapy on your own.
- Attend prenatal classes that discuss positioning your newborn.
- Attend newborn playgroups that promote prone play or tummy time.
What Kind of Physical Therapist Do I Need?
All physical therapists are trained through education and experience to evaluate, manage, and treat a variety of conditions, including torticollis. You may want to consider seeing:
- A pediatric physical therapist experienced in treating infants and children with torticollis.
- A physical therapist who is a board-certified clinical specialist in pediatric physical therapy, or who has completed a residency or fellowship in pediatric physical therapy. This physical therapist has advanced knowledge, experience, and skills that may apply to your baby’s condition.
You can find physical therapists in your area with these credentials and clinical expertise through Find a PT, a tool built by the American Physical Therapy Association.
General tips when you're looking for a physical therapist (or any other health care provider):
- Get recommendations from family, friends, or other health care providers.
- Ask about the physical therapist's experience treating torticollis before you make an appointment.
- Be prepared to describe your child's history since birth and their symptoms in as much detail as possible.
The APTA Academy of Pediatric Physical Therapy contributed to this consumer resource. It is for informational purposes only and is not intended to represent the position of APTA Pediatrics.
The American Physical Therapy Association believes that consumers should have access to information to:
- Inform their health care decisions.
- Prepare them for their visit with a health care provider.
The following resources offer some of the best scientific evidence related to physical therapy treatment for torticollis. They report recent research and provide information on the standards of practice in the United States and worldwide. They link to a PubMed* abstract (which may offer free access to the full text) or to other helpful resources. You can read them to learn more or bring a copy to your health care provider.
American Physical Therapy Association, ChoosePT. Tummy time: tips for parents. https://www.choosept.com/health-tips/tummy-time-tips-for-parents. Accessed June 16, 2022.
American Physical Therapy Association, ChoosePT. Physical therapy guide to head-shape flatness in infants. https://www.choosept.com/guide/physical-therapy-guide-to-head-shape-flatness-in-infants-plagiocephaly. Accessed June 16, 2022.
American Physical Therapy Association, ChoosePT. Health center for children. https://www.choosept.com/health-centers/children. Accessed June 16, 2022.
Hospital for Special Surgery. Physical therapy for muscular torticollis [video]. http://www.hss.edu/conditions_physical-therapy-for-muscular-torticollis.asp. Accessed June 16, 2022.
Pathways.org. Parents’ guide to tummy time [video]. https://pathways.org/topics-of-development/tummy-time/. Accessed June 6, 2022.
Medscape. Pediatric torticollis surgery. https://emedicine.medscape.com/article/939858-overview. Updated April 2, 2021. Accessed June 9, 2022.
Cunha B, Tadi P, Bragg BN. Torticollis. https://www.ncbi.nlm.nih.gov/books/NBK539857/. Updated September 9, 2021. Accessed June 16, 2022.
Kaplan SL, Coulter C, Sargent B. Physical therapy management of congenital muscular torticollis: a 2018 evidence-based clinical practice guideline from the APTA Academy of Pediatric Physical Therapy. Pediatr Phys Ther. 2018;30(4):240–290. Article Summary in PubMed.
Hu CF, Fu TC, Chen CY, Chen CP, Lin YJ, Hsu CC. Longitudinal follow-up of muscle echotexture in infants with congenital muscular torticollis. Medicine (Baltimore). 2017;96(6):e6068. Article Summary in PubMed.
Lee K, Chung E, Lee B-H. A comparison of outcomes of asymmetry in infants with congenital muscular torticollis according to age upon starting treatment. J Phys Ther Sci. 2017;29(3):543–547. Article Summary in PubMed.
Neumann, Donald A. Kinesiology of the Musculoskeletal System: Foundations for Physical Rehabilitation. St Louis, MO: Mosby Publishers; 2016.
Kaplan SL, Coulter C, Fetters L. Physical therapy management of congenital muscular torticollis: an evidence-based clinical practice guideline: from the Section on Pediatrics of the American Physical Therapy Association. Pediatr Phys Ther. 2013;25(4):348–394. Article Summary in PubMed.
Kim SN, Shin YB, Kim W, et al. Screening for the coexistence of congenital muscular torticollis and developmental dysplasia of hip. Ann Rehabil Med. 2011;35(4):485–490. Article Summary in PubMed.
Laughlin J, Luerssen TG, Dias MS. Prevention and management of positional skull deformities in infants. Pediatrics. 2011;128(6):1236–1241. Article Summary in PubMed.
Fradette J, Gagnon I, Kennedy E, Snider L, Majnemer A. Clinical decision making regarding intervention needs of infants with torticollis. Pediatr Phys Ther. 2011;23(3):249–256. Article Summary in PubMed.
Wen LM, Baur LA, Simpson JM, Rissel C. Flood VM. Effectiveness of an early intervention on infant feeding practices and "tummy time." Arch Pediatr Adolesc Med. 2011;165(8):701–707. Article Summary in PubMedArticle Summary in PubMed.
Koren A, Reece SM, Kahn-D'angelo L, Medeiros D. Parental information and behaviors and provider practices related to tummy time and back to sleep. J Pediatr Health Care. 2010;24(4):222–230. Article Summary in PubMed.
Öhman AM, Nilsson S, Beckung ER. Stretching treatment for infants with congenital muscular torticollis: physiotherapist or parents? A randomized pilot study. PM R. 2010;2(12):1073–1079. Article Summary in PubMed.
Stellwagen LM, Hubbard ET, Chambers C, Jones KL. Torticollis, facial asymmetry and plagiocephaly in normal newborns. Arch Dis Child. 2008;93(10):827–831. Article Summary in PubMed.
Hagan JF, Shaw JS, Duncan PM. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. 3rd ed. Elk Grove Village, IL: American Academy of Pediatrics; 2008.
Council on Children With Disabilities, Section on Developmental Behavioral Pediatrics, Bright Futures Steering Committee, Medical Home Initiatives for Children With Special Needs Project Advisory Committee. Identifying infants and young children with developmental disorders in the medical home: an algorithm for developmental surveillance and screening. Pediatrics. 2006;118(1):405–420. Article Summary in PubMed.
Tatli B, Aydinli N, Çaliskan M, Ozmen M, Bilir F, Acar G. Congenital muscular torticollis: evaluation and classification. Pediatr Neurol. 2006;34(1):41–44. Article Summary in PubMed.
Chen MM, Chang HC, Hsieh CF, et al. Predictive model for congenital muscular torticollis: analysis of 1021 infants with sonography. Arch Phys Med Rehabil. 2005;86(11):2199–2203. Article Summary in PubMed.
Stellwagen LM, Hubbard E, Vaux K. Look for the "stuck baby" to identify congenital torticollis. Contemp Pediatr. 2004;21(5):55–65.
Littlefield TR, Kelly KM, Reiff JL, Pomatto JK. Car seats, infant carriers, and swings: their role in deformational plagiocephaly. J Prosthet Orthot. 2003;15(3):102–106.
Sahrmann SA. Diagnosis and Treatment of Movement Impairment Syndromes. St Louis, MO: Mosby Publishers; 2002.
Cheng JC, Wong MW, Tang SP, Chen TM, Shum SL, Wong EM. Clinical determinants of the outcome of manual stretching in the treatment of congenital muscular torticollis in infants. A prospective study of eight hundred and twenty-one cases. J Bone Joint Surg Am. 2001;83(5):679–687. Article Summary in PubMed.
Hollier L, Jeong K, Grayson B, McCarthy J. Congenital muscular torticollis and this associated craniofacial changes. Plast Reconstr Surg. 2000;105(3):827–835. Article Summary in PubMed.
American Academy of Pediatrics, Committee on Pediatric Research. Race/ethnicity, gender, socioeconomic status-research exploring their effects on child health: a subject review. Pediatrics. 2000;105(6):1349–1351. Article Summary in PubMed.
Cheng JC, Metreweli C, Chen TM, Tang S. Correlation of ultrasonographic imaging of congenital muscular torticollis with clinical assessment in infants. Ultrasound Med Biol. 2000;26(8):1237–1241. Article Summary in PubMed.
Macdonald D. Sternomastoid tumour and muscular torticollis. J Bone Joint Surg Br. 1969;51(3):432–43. Article Summary in PubMed.
Tubby AH. Deformities and Diseases of Bones and Joints. 2nd ed. Vol. 1. London, United Kingdom: MacMillan; 1912:56.
*PubMed is a free online resource developed by the National Center for Biotechnology Information. PubMed contains millions of citations to biomedical literature, including citations in the National Library of Medicine's MEDLINE database.
Expert Review:
May 23, 2022
Revised:
Jun 17, 2022
Content Type: Guide
Torticollis
PT, PhD, board-certified clinical specialist in pediatric physical therapy
Elissa Derbak
PT, DPT, on behalf of the Academy of Pediatric Physical Therapy
You Might Also Like...
Health Tips
Tips to Select Toys for Children with Special NeedsSep 3, 2024
Play has an important role in the growth and development of children of all abilities, but it is particularly valuable for children with special needs
