Physical Therapy Guide to Hip Bursitis
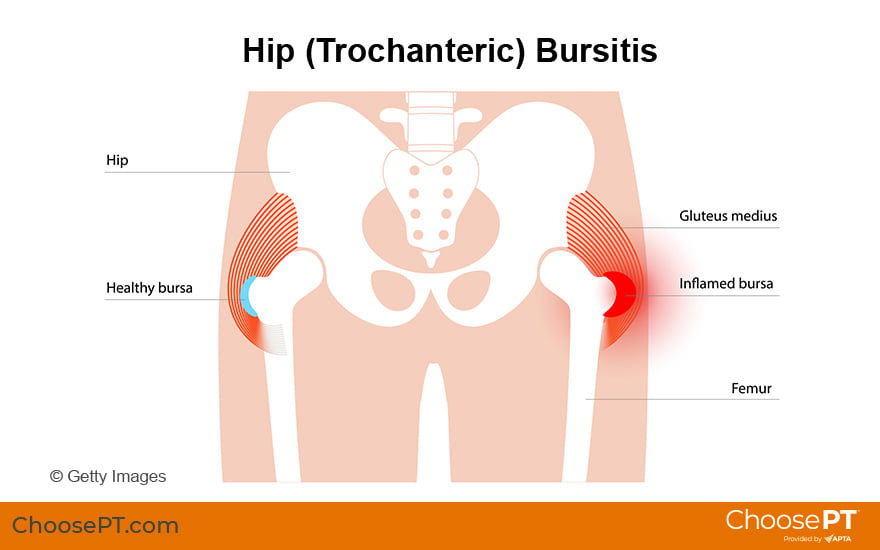
Hip bursitis is inflammation of the small fluid-filled sacs (bursae) that provide cushioning between the soft tissues of the hip (muscles, tendons, and ligaments), and the hip bones. Most commonly, bursitis causes pain at the hip joint that extends to the outside of the thigh area. Hip bursitis, located on the outside of the hip, is called greater trochanteric bursitis. Bursitis can affect anyone. It is more common in middle-aged and older adults and affects women more often than men. Hip bursitis often results due to repeated stress (overuse) from activities or sports that produce tension or friction in the hip. Physical therapists can effectively treat hip bursitis. They work with people to reduce pain and irritation and help them get back to everyday activities. Physical therapists also address any related weakness in the hip, back, or lower extremity that may contribute to the condition.
Physical therapists are movement experts. They improve quality of life through hands-on care, patient education, and prescribed movement. You can contact a physical therapist directly for an evaluation. To find a physical therapist in your area, visit Find a PT.
What Is Hip Bursitis?
Bursitis at the outer (lateral) side of the hip is called greater trochanteric bursitis or hip bursitis. It occurs when the bursa on the outside of the hip becomes damaged, irritated, or inflamed. A bursa is a fluid-filled sac that provides a cushion between the hip bones and the muscles, tendons, and ligaments during movement. “Itis” means "inflammation.” The irritated and inflamed bursa causes pain that can limit range of motion and make some activities or positions uncomfortable.
Certain positions, motions, or diseases can cause friction or stress on the bursa, and lead to bursitis. When the bursa becomes injured, muscles and tendons do not glide smoothly, which can result in pain.
Hip bursitis develops as a result of repeated irritation in the hip. It seldom results from a single injury. Hip bursitis can be caused by:
- Repeated motions that irritate the bursa (such as walking, running on hills or uneven surfaces, or stair climbing).
- Abnormal walking due to injury, leg length differences, or problems in the spine.
- Muscle weakness.
- Incorrect posture.
- Hip surgery or replacement.
- Bone spurs in the hip.
- Infection.
- Autoimmune diseases, such as rheumatoid arthritis, gout, psoriasis, or thyroid disease.
- Direct trauma (being hit or falling on the side of the hip).
Trochanteric bursitis is the main form of hip bursitis. A less common form (ischial bursitis) occurs at the pelvic bone. Ischial bursitis causes pain at the groin and back of the hip, rather than at the side.
How Does It Feel?
With hip bursitis, the main symptom you may experience is pain on the outer side of the hip, thigh, buttock, or outside of the leg. That pain can worsen when getting up from sitting, such as from a low chair or car seat. Pain can also be triggered by:
- Pushing on the outer side of the hip with your fingers.
- Lying on the affected hip.
- Climbing stairs.
- Walking or running.
- Lifting the leg up to the side.
- Sitting with crossed legs.
How Is It Diagnosed?
Your physical therapist will conduct a full evaluation and physical exam to assess the degree of your condition and determine the cause and contributing factors to it. They will begin by gathering information about your condition, including your health history and your current symptoms. They will then examine your hip and thigh region to determine the presence and type of bursitis. Your physical therapist may ask you questions about:
- Your health history.
- Your current symptoms and how they may affect your typical day.
- The location and intensity of your pain, and how it may vary during the day.
- How the pain affects your activity level, and what you do to reduce the pain.
- How any injury may have occurred prior to your symptoms developing.
- How you have sought treatment, such as seeing other health care practitioners or having imaging or other tests done.
Your physical examination will focus on the region of your symptoms. It also will include other areas that may have been affected as your body has adjusted to avoid the pain. Your physical therapist may watch you walk, step onto a stair, squat, or balance on one leg. Based on the findings of your exam, your physical therapist will develop a personalized treatment program to address your specific condition and goals.
Imaging, such as X-ray or MRI, are typically not needed to diagnose bursitis.
How Can a Physical Therapist Help?
Your physical therapist will work with you to design a specific treatment program that will speed your recovery. This program will include exercises and treatments that you can do at home. Physical therapy will help you return to your normal lifestyle and activities. The time it takes to heal the condition varies on your age and condition. Results often can be achieved in several weeks, when following a proper stretching and strengthening program.
As part of your treatment, your physical therapist will work with you to:
Reduce pain and swelling. Your physical therapist will teach you how to avoid or modify certain activities to promote healing. They may use special treatments and technologies to control and reduce your pain and swelling. These may include ice, heat, ultrasound, electrical stimulation, taping, and specific exercises. They also may use hands-on therapy, such as massage.
Improve motion. Your physical therapist will choose specific activities and treatments to help restore normal movement in your hip and leg. These might begin with "passive" motions that the physical therapist performs for you to gently move your hip joint. At the right time, you will progress to doing active exercises and stretches that you do yourself.
Improve flexibility. Your physical therapist will determine if any leg or spinal muscles are tight. They will help you to stretch the muscles and teach you how to stretch them on your own.
Improve strength. Hip bursitis is often related to weak or injured hip muscles. Certain exercises will aid healing at each stage of recovery. Your physical therapist will teach you the correct exercises to steadily restore your strength and agility. They may have you use cuff weights, stretch bands, weightlifting equipment, and cardio-exercise equipment, such as treadmills or stationary bicycles.
Improve balance. Regaining your sense of balance is important after an injury. Your physical therapist will teach you exercises to improve your balance skills.
Learn a home exercise program. Your physical therapist will design a home exercise program and teach you strengthening and stretching exercises to do at home. These exercises will be specific for your needs. Following your home exercise program as prescribed by your physical therapist can speed your recovery.
Return to activities. Your physical therapist will discuss your activity goals with you. They will work with you to set work, sport, and home-life recovery goals. Your treatment program will help you reach your goals in the safest, fastest, and most effective way possible. They also may use work retraining activities and sport-specific drills to help you return to the activities you enjoy.
If Surgery Is Needed
Surgery is rarely needed for hip bursitis. If it is, you will follow a recovery program over several weeks. Your program will include some or all of the elements listed above, tailored to your specific condition and goals. Your physical therapist will address your pain. They also will help you safely regain motion and strength so you can return to your normal activities as quickly as possible.
Can This Injury or Condition Be Prevented?
Hip bursitis cannot always be prevented. You can, however, avoid activities that make it worse or put you at risk for reinjury. Your physical therapist can recommend exercises to strengthen and stretch the muscles around your knee, upper leg, and abdomen to help prevent bursitis from recurring. These may include strength and flexibility exercises for the leg, knee, and core muscles.
To help prevent a recurrence of the injury, your physical therapist may advise you to:
- Follow a consistent flexibility and strengthening exercise program. It is important to maintain good physical condition of your hip muscles. This is especially true for athletes in a sport's off-season.
- Always warm up before starting a sport or heavy physical activity.
- Only increase activity gradually. A sudden increase in activity or intensity is a frequent cause of injury.
- Get and wear properly fitted shoes, and use a shoe insert to address any difference in leg length.
- Learn and maintain correct posture.
What Kind of Physical Therapist Do I Need?
All physical therapists are prepared through education and experience to treat hip bursitis. However, you may want to consider:
- A physical therapist who is experienced in treating people with muscle, bone, and joint (musculoskeletal) injuries. Some physical therapists have a practice with an orthopedic or sports focus.
- A physical therapist who is a board-certified clinical specialist, or who completed a residency or fellowship in orthopedic or sports physical therapy. This physical therapist has advanced knowledge, experience, and skills that may apply to your condition.
You can find physical therapists in your area with these credentials and clinical expertise on Find a PT, a tool built by the American Physical Therapy Association.
General tips when you are looking for a physical therapist (or other health care provider):
- Ask family, friends, and other health care providers to recommend a physical therapist.
- Ask about the physical therapist’s experience treating hip bursitis before you make an appointment.
- Be prepared to describe your symptoms in as much detail as possible on your first visit, including what makes your symptoms better or worse.
The American Physical Therapy Association believes that consumers should have access to information to:
- Inform their health care decisions.
- Prepare them for their visit with a health care provider.
The following resources offer some of the best scientific evidence related to physical therapy treatment for hip bursitis. They report recent research and provide information on the standards of practice in the United States and internationally. They link to a PubMed* abstract (which may offer free access to the full text) or other resources. You can read them to learn more or bring a copy to your health care provider.
Disantis AE, Martin RL. Classification Based Treatment of Greater Trochanteric Pain Syndrome (GTPS) with Integration of the Movement System. Int J Sports Phys Ther. 2022 Apr 1;17(3):508-518. Article Summary on PubMed.
Marín-Pena O, Papavasiliou AV, Olivero M, Galanis N, Tey-Pons M, Khanduja V. Non-surgical treatment as the first step to manage peritrochanteric space disorders. Knee Surg Sports Traumatol Arthrosc. 2021;29(8):2417-2423. Article Summary on PubMed.
Pianka MA, Serino J, DeFroda SF, Bodendorfe BM. Greater trochanteric pain syndrome: evaluation and management of a wide spectrum of pathology. Article Summary on PubMed.
*PubMed is a free online resource developed by the National Center for Biotechnology Information. PubMed contains millions of citations to biomedical literature, including citations in the National Library of Medicine’s MEDLINE database.
Expert Review:
May 10, 2022
Revised:
Aug 31, 2022
Content Type: Guide
Hip Bursitis
PT, DPT
Stephen F. Reischl
PT, DPT, board-certified clinical specialist in orthopaedic physical therapy, on behalf of the Academy of Orthopaedic Physical Therapy
You Might Also Like...
Video
Physical Therapy Helps Senior Games Athlete Return to the Basketball CourtOct 30, 2019
William is a former Senior U.S. Olympic team athlete who stopped playing basketball due to hip pain. Physical therapy helped to eliminate his pain, and
