Physical Therapy Guide to Herniated Disk
A herniated disk occurs when a disk between the bones of the spine is injured. This can be caused by sudden trauma or long-term pressure on the spine. The condition most often affects people ages 30 to 50 years. Men are twice as likely to be diagnosed as women. Repeated lifting, heavy weight-bearing sports, obesity, smoking, and excessive sitting are all risk factors for a herniated disk. The majority of herniated disks respond best to physical therapy and do not require surgery. Physical therapists personalize treatment programs to help people with herniated disks regain normal movement, reduce pain, and get back to their regular activities.
Physical therapists are movement experts. They improve quality of life through hands-on care, patient education, and prescribed movement. You can contact a physical therapist directly for an evaluation. To find a physical therapist in your area, visit Find a PT.
What Is a Herniated Disk?
The spine is made up of 33 bones called vertebrae stacked on top of each other. Between each vertebra is a cushion-like structure called a “disk." A herniated disk occurs when the inner part of the disk, which is softer and more mobile, is displaced toward its outer portion. Let’s review the anatomy of the disk.
- The outer portion of the disk is called the annulus fibrosus, made up of layers of strong tissues (laminae) that help control movements of the spine.
- The inner portion of the disk, called the nucleus pulposus, is a softer, toothpaste-like substance that is uniquely designed to provide the spine with mobility while also helping the spine absorb and withstand pressure.
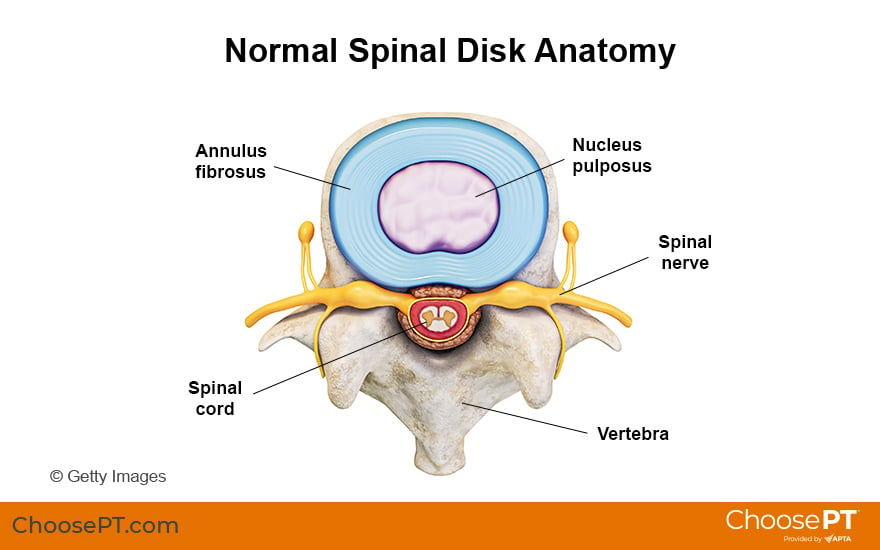
A spinal disk is strong, flexible, and absorbs shock extremely well. As people age, however, disks can lose some flexibility, and the risk for tearing increases. A herniated disk is when the toothpaste-like center portion (nucleus pulposus) displaces or pushes outward through a tear in the disk’s tougher outer layer. In more severe cases, the herniation can eventually press on nearby nerves or the spinal cord, causing nerve pain or injury.
Injuries that cause herniation can occur rapidly or develop slowly over time.
- A sudden injury can occur when an individual lifts something while in a poor position. Athletes competing in weight-bearing sports, such as weightlifting, also can cause injury with incorrect movements. These actions strain the spine and cause a sudden tear in the outer part of a disk.
- A slow injury can occur as the result of sitting or standing with poor posture (slumped forward) for hours, weeks, or years, slowly overstretching or tearing the outer part of a disk.
The most common area of the spine to experience a herniated disk is the lower back, just below the waist level. Herniated disks also commonly occur in the neck.
In people older than 50, the disk can become even more stiff, making it less likely to herniate. This change, however, can lead to other conditions that cause pain and stiffness, such as degenerative disk or joint disease. Your physical therapist will work with your other health care providers to determine your correct diagnosis.
How Does It Feel?
Symptoms linked to a herniated disk can vary. Pain often occurs across the entire lower back. If a nerve is involved, it can cause numbness, weakness, or tingling in the neck, back, arms, or legs. It is important to remember that pain in the lower back can be caused by structures other than the disk. Some people may feel no pain with a herniated disk. An evaluation by a physical therapist can help determine the cause of your pain and rule out other conditions.
With severe pressure on a nerve or on the spinal cord, surgery may be needed to immediately relieve that pressure. Your physical therapist can help determine whether either of these conditions is occurring. They will work closely with your physician and surgeon to determine the correct treatment.
Signs and Symptoms
The type and location of symptoms will depend on the level of the disk herniation (which vertebra the problem is between) and the direction of the protrusion, such as back and toward the left or back and toward the right. Symptoms also depend on the amount of pressure on nearby nerves.
A herniated disk may cause no pain at all. Or it can cause any of the following symptoms:
- Pain in the neck, back, lower back, arms, or legs
- Inability to bend or rotate the neck or back
- Numbness or tingling in the neck, shoulders, arms, hands, hips, legs, or feet
- Weakness in the arms or legs
- Limping when walking
- Increased pain when coughing, sneezing, reaching, or sitting
- Inability to stand up straight; being "stuck" in a position, such as being stooped forward or leaning to the side
- Difficulty getting up from a chair
- Inability to remain in one position for long periods, such as sitting or standing, due to pain
- Pain that is worse in the morning
How Is It Diagnosed?
Your physical therapist will conduct a thorough evaluation that includes taking your health history. They also will ask you detailed questions about your injury, such as:
- How and when did the pain start?
- Does the pain change throughout the day?
- What type of discomfort do you feel, and where do you feel it?
- What can’t you do right now, in your daily life, due to the pain?
Your physical therapist will perform tests on your body to find physical problems, such as:
- Difficulty moving
- Weakness or tightness in the muscles
- Loss of skin sensation in some areas (numbness)
- Loss of reflexes
- Joint stiffness
- Poor posture
- Difficulty walking
If your physical therapist finds any of the above problems, you may begin physical therapy right away to help get you on the road to recovery.
If testing identifies more severe problems, your physical therapist may work with your physician or surgeon to obtain special diagnostic testing, such as an MRI. Physical therapists work closely with your other health care providers to ensure that you receive an accurate diagnosis and the treatment and care you need.
How Can a Physical Therapist Help?

In all but the most extreme cases, conservative care (such as physical therapy) often produces better results in treating a herniated disk than surgery or pain medications, such as opioids.
Your physical therapist will work with you to design a specific treatment program that will speed your recovery. This can include exercises and treatments that you can do at home in between clinic visits. Physical therapy will help you return to your normal lifestyle and activities. Healing and recovery time varies. Patients who follow a personalized physical therapy plan, including a proper postural, pain-reduction, stretching, and strengthening program, typically see improvement in a few weeks.
First 24 to 48 Hours
During the first 24 to 48 hours following your diagnosis of a herniated disk, your physical therapist may advise you to:
- Avoid too much rest and/or any activity that causes worsening symptoms in the back, arms, or legs.
- Stay active around the house, and go on short walks several times per day. Movement will decrease pain and stiffness and help you feel better.
- Apply ice packs to the affected area for 15 to 20 minutes every 2 hours.
- Sit in firm chairs. Soft couches and easy chairs may make your problems worse. Your physical therapist may recommend that you stand up and move every 30 minutes. You may also use a small pillow placed in the lower part of your back when sitting or driving.
Treatment Program
Your physical therapist will design a personalized exercise program to meet your specific needs. Certain exercises may be better for you than others. For example:
- Exercising in water can be a great way to stay physically active when other forms of exercise are painful.
- Exercises that involve twisting and bending may or may not benefit you.
- Weight-training exercises, although very important, need to be done with proper form to avoid stress to the back and neck.
- A walking program to gradually improve your tolerance to activity.
Your physical therapist will work with you to:
Reduce pain and other symptoms. Your physical therapist will help you understand how to avoid or modify the activities that caused your injury. They may use different types of treatments and technologies to control and reduce your pain and symptoms.
Improve posture. If your physical therapist finds that poor posture has contributed to your herniated disk, they will teach you how to improve your posture. This will reduce pressure in the injured area. With proper treatment, healing can begin and progress as safely and quickly as possible.
Improve motion. Your physical therapist will choose specific activities and treatments to help restore normal movement in any stiff joints. These might begin with "passive" motions that the physical therapist performs for you to move your spine. They may progress to “active” exercises and stretches that you do yourself. You can do these movements and exercises at home and at work throughout the day to help speed your recovery.
Improve flexibility. Your physical therapist will determine if any of the involved muscles are tight. They can help you stretch them and teach you how to stretch them at home.
Improve strength. If your physical therapist finds any weak or injured muscles, they will select and teach you the right exercises to restore your strength and agility. For neck and back disk herniations, “core strengthening” is commonly used. This helps restore the strength and coordination of muscles around your back, hips, abdomen, and pelvis.
Improve endurance. Restoring muscular endurance is important after any injury. Your physical therapist will develop a program of activities to help you regain the endurance you had before the injury and improve it.
Learn a home program. Your physical therapist will teach you strengthening, stretching, and pain-reduction exercises to do at home. These exercises will be specific to your needs. If you do them as prescribed, you can speed your recovery.
Return to activities. Your physical therapist will discuss your activity level with you and help you set your work, sport, and home-life recovery goals. Your treatment program will help you reach your goals in the safest, fastest, and most effective way possible. For spine injuries like a herniated disk, your physical therapist may teach you proper “body mechanics” — correct ways to do daily tasks and lift heavy objects. This can help protect your spine from further injury.
Once you are pain-free, it will still be important to continue the exercises and other recommendations provided by your physical therapist to keep your back healthy and strong.
Following Surgery
In rare cases, surgery is necessary to prevent permanent damage to a nerve or the spinal cord. If you undergo surgery for your herniated disk, your physical therapist will work closely with you and your surgeon to help you regain motion and strength more quickly than you could on your own. They can help you get back to your normal lifestyle as safely and quickly as possible.
Can This Injury or Condition Be Prevented?
To prevent experiencing a herniated disk, individuals should:
- Use proper body mechanics when lifting, pushing, pulling, or performing any action that puts extra stress on your spine.
- Maintain a healthy weight. This will reduce the stress on your spine.
- Stop smoking.
- Discuss your occupation with a physical therapist. They can provide an analysis of your job tasks and offer suggestions for reducing your risk of injury.
- Keep your muscles strong and flexible. Participate in a consistent program of physical activity to maintain a healthy fitness level.
Many physical therapy clinics offer "back schools," which teach people how to take care of their backs and necks and prevent injury. Ask your physical therapist about programs in your area. If you don't have a physical therapist, the American Physical Therapy Association provides Find a PT to help you find a licensed physical therapist in your area.
To prevent recurrence of a herniated disc, follow the above advice and:
- Continue the new posture and movement habits that you learned from your physical therapist.
- Continue to do the home-exercise program your physical therapist taught you. This will help maintain your improvements.
- Continue to be physically active and stay fit.
What Kind of Physical Therapist Do I Need?
All physical therapists are prepared through education and experience to treat people who have a herniated disk and resulting pain. You may want to consider:
- A physical therapist who is experienced in treating people with orthopedic, or musculoskeletal, problems.
- A physical therapist who is a board-certified clinical specialist or who completed a residency or fellowship in orthopedic physical therapy. This physical therapist has advanced knowledge, experience, and skills that may apply to your condition.
You can find physical therapists who have these and other credentials by using Find a PT, the online tool built by the American Physical Therapy Association to help you search for physical therapists with specific clinical expertise in your geographic area.
General tips when you’re looking for a physical therapist:
- Get recommendations from family, friends, or other health care providers.
- Ask about the physical therapists’ experience in helping people with a herniated disk.
- Be prepared to describe your symptoms in as much detail as possible and say what makes your symptoms worse.
The American Physical Therapy Association believes that consumers should have access to information that can help:
- Inform their health care decisions.
- Prepare them for their visit with a health care provider.
The following resources offer some of the best scientific evidence related to physical therapy treatment for a herniated disk. They report recent research and provide information on the standards of practice in the United States and internationally. They link to a PubMed* abstract (which may offer free access to the full text) or other resources. You can read them to learn more or bring a copy to your health care provider.
El Melhat AM, Youssef ASA, Zebdawi MR, et al. Non-surgical approaches to the management of lumbar disc herniation associated with radiculopathy: a narrative review. J Clin Med. 2024;13(4):974. Article Summary in PubMed
Zhou M, Theologis AA, O'Connell GD. Understanding the etiopathogenesis of lumbar intervertebral disc herniation: From clinical evidence to basic scientific research. JOR Spine. 2023;7(1):e1289. Article Summary in PubMed
Swanson BT, Creighton D. Cervical disc degeneration: important considerations for the manual therapist. J Man Manip Ther. 2022;30(3):139–153. Article Summary in PubMed
George SZ, Fritz JM, Silfies SP, et al. Interventions for the management of acute and chronic low back pain: revision 2021. J Orthop Sports Phys Ther. 2021;51(11):CPG1–CPG60. Article Summary in PubMed
Yang X, Karis DSA, Vleggeert-Lankamp CLA. Association between Modic changes, disc degeneration, and neck pain in the cervical spine: a systematic review of literature. Spine J. 2020;20(5):754–764 Article Summary in PubMed
Desmoulin GT, Pradhan V, Milner TE. Mechanical aspects of intervertebral disc injury and implications on biomechanics. Spine (Phila Pa 1976). 2020;45(8):E457–E464. Article Summary in PubMed
Expert Review:
Dec 7, 2024
Revised:
Apr 1, 2025
Content Type: Guide
Herniated Disk
PT, DPT, Board-Certified Clinical Specialist in Orthopaedic Physical Therapy
PT, DPT, Board-Certified Clinical Specialist in Orthopaedic Physical Therapy
PT, DPT, Board-Certified Clinical Specialist in Orthopaedic Physical Therapy
PT, DPT, ATC, Board-Certified Clinical Specialist in Orthopaedic Physical Therapy
Laura Thornton
Board-Certified Clinical Specialist in Orthopaedic Physical Therapy, and Fellow of the American Academy of Orthopaedic Manual Physical Therapy, on behalf of the Academy of Orthopaedic Physical Therapy
You Might Also Like...
Podcast
Success Story: Avoiding Back Surgery to Return to MarathonsNov 20, 2014
Andrea Parada ran her first marathon in her 40s without pain. Months later, she could hardly get out of bed.