Physical Therapy Guide to Flat Head Syndrome: Plagiocephaly, Brachycephaly, and Dolichocephaly
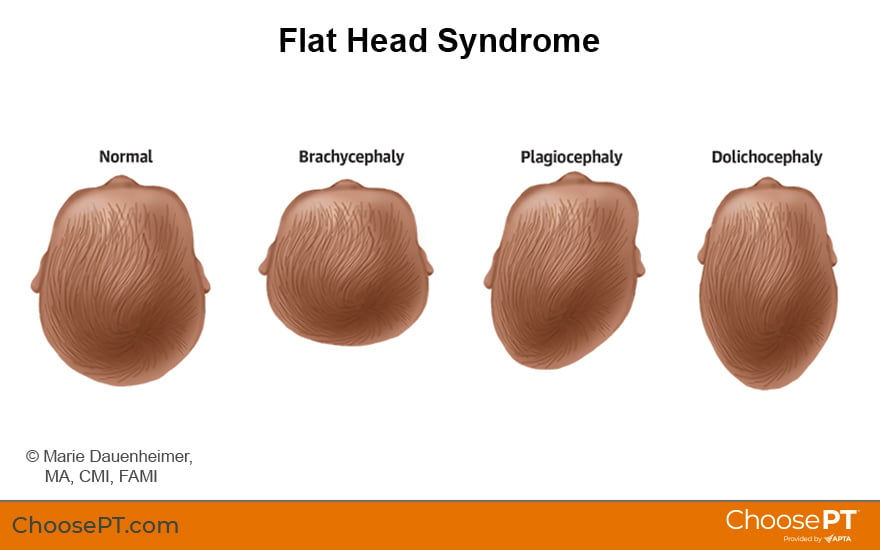
Infant flat head syndrome is an atypical flattening or deformation of the skull that may present as:
- Plagiocephaly (back of the head is flat on one side in a "slant").
- Brachycephaly (flat across the back of the head on both sides).
- Dolichocephaly (flat on the sides of the head and the head is elongated front to back).
The main cause of flat head syndrome is the baby's positioning within their environment. Before birth, skull flattening can occur if the baby is stuck in a tight position in the womb. The condition occurs more commonly in pregnancy with multiple babies (twins, triplets) or a mother's first pregnancy. After birth, a baby's positioning during wake time and sleep also can cause changes in head shape.
Physical therapists help determine the cause of the head flattening and the best treatment. A referral to another specialist also may be recommended. The sooner a family sees a physical therapist, the better the chances of improving or preventing further head shape deformities. Early physical therapy also helps to reduce the risk for related developmental problems.
Physical therapists are movement experts who use the latest evidence to design treatment plans for each person's needs and goals. They improve quality of life through hands-on care, patient education, and prescribed movement. You can contact a physical therapist directly for an evaluation.
To locate a physical therapist near you, visit Find a PT.
What Is Flat Head Syndrome?
Plagiocephaly, brachycephaly, and dolichocephaly are different types of infant flat head syndrome.
These shape types are caused by external forces on the baby's head before or after birth. Before birth, the baby's position in the womb (often due to shared space with multiple babies) can put pressure on the skull. After birth, a baby's positioning during sleep or wake time may lead to too much time spent with pressure on one area of a baby's soft skull.
Plagiocephaly is the most common type of infant flat head syndrome. Generally, the back of the baby's head is flat on one side. The baby may prefer to keep their head turned consistently to one side. Plagiocephaly can result from a tight muscle (as with torticollis), the baby's visual preference, or because gravity leads them to turn and rest on the flat side, especially if a flat spot was present at birth. Often parents will be the first to notice the flat spot. Without intervention, the flattening may worsen. This can cause the ear, forehead, and jaw on the same side to shift forward from their typical position.
Brachycephaly is the second most common type of flat head syndrome. The back of the head is flattened instead of curved. This is often caused because the child spends too much time lying on their back or in equipment such as car seats or swings. Brachycephaly can cause the head shape to widen, and the ears may cup or roll forward due to the pressure on the skull bones.
Dolichocephaly is the flattening of the head from side to side. It is common in the womb with:
- Breech positioning (the baby is "feet down" in the womb in the last trimester rather than the expected "head down" position).
- Frank breech positioning ("bottom down," but with the knees extended and feet up by the head).
It also can occur if the head is often positioned side to side for long periods. This sometimes occurs with premature babies who spend time in a neonatal intensive care unit. Improvements in positioning babies during their time in the NICU have decreased the number of cases with this head shape.
Scaphocephaly, a subtype of head flattening, falls under the umbrella of dolichocephaly since it is the same elongated head shape. The cause is a more serious congenital condition called sagittal craniosynostosis, an early closure of the suture (seam) on top of the skull that runs from front to back.
Since the early 1990s, the number of cases of flat head syndrome has grown dramatically. Major factors contributing to the increase include the following changes in the modern infant's environment:
- The American Academy of Pediatrics' "Back to Sleep" campaign encouraged parents to place babies on their backs to sleep. The campaign, which started in 1992, lowered the rate of sudden infant death syndrome by 50%. However, an associated increase in the rate of infants with head shape flatness was noted. The updated campaign, Safe Sleep, continues to recommend that babies be placed on their backs to sleep to reduce the risk of SIDS. However, babies should have ample "tummy time" while awake.
- Babies started spending less time (on average 0 to 15 minutes daily) on their tummies due to fear of SIDS. Babies should spend several periods on their tummy with a caregiver present to add up to at least one hour each day.
- Parents increased their use of infant containers, such as swings, bouncy chairs, and portable car seats. As a result, more babies spend long periods on their backs or in semi-upright positions (up to 20 hours per day).
Doctors and pediatric physical therapists began noticing changes in infant motor development. They also saw increased numbers of infants with flat spots on the head. Parents often noted a flat skull even before discovering their child preferred to hold their head to one side.
Signs and Symptoms
The following conditions also may be present with flat head syndrome:
- Torticollis. This is a condition in which the baby tips their ear toward one shoulder and/or keeps their face turned toward the opposite shoulder. It is due to a tight neck muscle or a flat skull. The facial muscles and bones also may be smaller on the tight side (the one they tip their ear toward).
- Facial asymmetry. The sides of the baby's face may appear unequal or uneven. The jaw may appear to be more forward on the flattened side.
Head shape deformities, especially if left untreated, can lead to:
- Feeding issues (the baby may not latch on to the breast or bottle initially and may have trouble transitioning to solid foods or textures).
- Speech and language delays.
- Visual problems, including a limited field of vision (by 20 degrees or more).
- Delayed cognitive (thinking and learning) and motor (movement) skills development.
- Balance problems.
- Attention deficit disorder and attention deficit and hyperactivity disorder.
- Poor fit of sports helmets.
- Poor fit of eyewear.
- Structural and functional changes in the brain.
How Is It Diagnosed?
Parents may notice that the baby's skull appears flattened on the back or side. They also may notice their baby keeps their head tilted and/or turned to one side more than the other.
Parents should be educated before and after the baby's birth and encouraged to seek an evaluation with a pediatric physical therapist, especially if they notice head flattening before the pediatrician.
The American Academy of Pediatrics recommends pediatricians screen infants for postural problems at every well-child visit from birth through six months.
- The pediatrician should rule out craniosynostosis.
- Infants with any uneven postures or positions should be referred to a pediatric physical therapist for evaluation as soon as flattening is noticed; do not wait until the next well visit.
As movement and developmental experts, pediatric physical therapists have the expertise and experience to properly screen, evaluate, and diagnose posture and skeletal imbalances. Ideally, all newborns should be screened by a physical therapist at birth and assessed yearly until they are young adults. These regular assessments can help to maximize healthy movement experiences throughout life.
How Can a Physical Therapist Help?
Your child's physical therapist will conduct a full evaluation. This will include taking the baby's birth and health history. They will ask you detailed questions about:
- Who provides most of the baby's care, whether at home or day care.
- How your baby is held, where they sleep, and their positioning throughout each day.
- Your baby's activity level.
Your child's physical therapist will examine and note:
- Skull shape and face symmetry. They may take pictures from various angles and positions and use a tool to take measurements.
- Muscle development, including your baby's movement and motion.
- Body position and the position of their arms, legs, and head while lying on their back and their tummy.
- Mobility, including their ability to roll over, crawl, and change positions.
- Reaching and holding skills.
- Ability to look at and follow objects with their eyes and head.
- Responses to sounds and the direction from which the sound is coming.
- Play and exploration skills.
- Responses to movement.
Pediatric physical therapists educate caregivers during all phases of infant development — during pregnancy, right after birth, or in the first few months. Early caregiver education will include tips for proper positioning and ways to create movement opportunities for your baby. This information is key to prevention, treatment, and avoiding a worsening of flat head syndrome or possible developmental problems. Education will include information on:
- Skull shape. Your child's physical therapist will inform you about the causes, progression, and effects of a flattened skull. They will teach you ways to solve positioning problems throughout the day and night and adapt the baby's environment to remove and avoid increased pressure on the flattened areas of their skull. Recommendations will include:
- Decreasing the amount of time your baby spends in infant containers.
- Increasing the time your baby spends in positions other than on their back (such as supervised tummy time or being held by an adult).
- Movement. Your physical therapist will educate you about any limitations in your baby's neck range of motion when turning and tipping side to side. They also will teach you various ways to position them to stretch the tight muscles and encourage movement toward their nonpreferred side.
- Strength. Babies need to have equal strength on both sides of their neck to develop normally. Your physical therapist will teach you ways to use toys, play, or songs to encourage new movements and ensure your baby develops equal strength on both sides.
Your child's physical therapist also may team up with the baby's primary care provider or other health care professionals on diagnosis and treatment options. Further assessments or specialists may be needed to confirm or rule out other diagnoses.
Your child's physical therapist may refer your baby to an orthotist to receive a head scan. Orthotists use various tools to aid diagnosis and monitor head shape changes. Tools may include digital imaging cameras, laser or handheld scanners, and an index for measuring the shape of the skull. None of these tools are harmful to the baby. Your physical therapist will help you with the process of obtaining a head scan and custom helmet (cranial orthosis) if needed to correct your baby's head shape.
Can This Injury or Condition Be Prevented?
There is no way to prevent congenital (developed in the womb before birth) flat head syndrome. The sooner a baby sees a pediatric physical therapist, the more likely it is to prevent further loss of range of motion or a worsening of the flattened skull. Early diagnosis at or shortly after birth provides the quickest and best results to help correct head shape flatness.
Correct positioning and regularly changing a baby's environment are keys to preventing acquired (after birth) flat head syndrome. Caregivers can do the following to create the best developmental environment for their baby:
- Position the baby to avoid pressure on the flat spot at all awake times.
- Increase supervised tummy time play starting at birth. Babies should get a minimum of 5-10 minutes of supervised tummy time at least five times per day and build up to the baby tolerating 30-60 minutes or more.
- Carry or hold the baby in your arms or use a wearable baby carrier in ways that avoid pressure on the flattened areas of their skull.
- Limit car seat use to during travel times only.
- Limit time in all infant containers (seats, bouncers, jumpers, swings) to no more than one to two times per day for a maximum of 15 minutes each time.
- Change the baby's position often.
- Change the "head of the bed" direction in the baby's crib or bassinet day to day or sleep to sleep. This will encourage your baby to turn their head to the nonpreferred side.
Families and caregivers should seek early screening of their newborns for any neck range of motion problems and a flat spot on the baby's skull. The sooner a baby sees a pediatric physical therapist, the sooner prevention or correction of muscle tightness and flattening of the skull can occur.
The following tips can help you ensure your baby has a healthy environment in which to grow and develop:
- Discuss any concerns with your child's pediatrician during well-baby visits.
- Ask for a referral to physical therapy or make an appointment to see a physical therapist directly.
- Attend prenatal classes that discuss positioning your newborn.
- Attend newborn playgroups that promote healthy movement and tummy time.
What Kind of Physical Therapist Do I Need?
All physical therapists are prepared through education and experience to treat a variety of conditions, including infant flat head syndrome. You may wish to consider:
- A pediatric physical therapist who is experienced in treating babies with flat head syndrome.
- A physical therapist who is a board-certified clinical specialist in pediatric or neurologic physical therapy. This physical therapist has advanced knowledge, experience, and skills for this condition.
You can find physical therapists in your area with these credentials and clinical expertise through Find a PT, a tool built by the American Physical Therapy Association.
General tips when looking for a physical therapist (or any other health care provider):
- Get recommendations from family, friends, or other health care providers.
- Ask about the physical therapist's experience treating flat head syndrome before making an appointment.
- Be prepared to describe your child's history since birth and their symptoms in as much detail as possible.
The Academy of Pediatric Physical Therapy contributed to this consumer resource. It is for informational purposes only and is not intended to represent the position of APTA Pediatrics.
Further Reading
The American Physical Therapy Association believes that consumers should have access to information to:
- Inform their health care decisions.
- Prepare them for their visit with a health care provider.
Hospital for Special Surgery. Physical therapy for muscular torticollis and plagiocephaly. Accessed June 8, 2022.
Pathways.org. Tummy Time. Accessed June 8, 2022.
ChoosePT.com. Tummy Time Tips for Parents c. American Physical Therapy Association. Accessed June 8, 2022.
ChoosePT.com. Physical Therapy Guide to Torticollis. ChoosePT.com. American Physical Therapy Association. Accessed June 8, 2022.
American Academy of Pediatrics. Safe sleep campaign. https://www.aap.org/en/news-room/campaigns-and-toolkits/safe-sleep/https://www.aap.org/en/news-room/campaigns-and-toolkits/safe-sleep/. Accessed June 6, 2022.
The following resources offer some of the best scientific evidence related to physical therapy treatment for head shape flatness in children. They report recent research and provide information on the standards of practice in the United States and internationally. They link to a PubMed* abstract (which may offer free access to the full text) or other resources. You can read them to learn more or bring a copy to your health care provider.
Collett BR, Wallace ER. Infant/toddler motor skills as predictors of cognition and language in children with and without positional skull deformation. Childs Nerv Syst. 2019;35(1):157–163. Article Summary in PubMed.
Collett BR, Wallace ER, Kartin D, Cunningham ML, Speltz ML. Cognitive outcomes and positional plagiocephaly. Pediatrics. 2019;143(2):e20182373. Article Summary in PubMed.
Kaplan SL, Coulter C, Sargent B. Physical therapy management of congenital muscular torticollis: a 2018 evidence-based clinical practice guideline from the APTA Academy of Pediatric Physical Therapy. Pediatr Phys Ther. 2018;30(4):240–290. Article Summary in PubMed.
Leung A, Mandrusiak A, Watter P, Gavranich J, Johnston LM. Impact of parent practices of infant positioning on head orientation profile and development of positional plagiocephaly in healthy term infants. Phys Occup Ther Pediatr. 2018;38(1):1–14. https://pubmed.ncbi.nlm.nih.gov/28375778/.
Sahrmann S. The how and why of the movement system: as the professional identity of physical therapy. Int J Sports Phys Ther. 2017;12(6):862–869. Article Summary in PubMed.
Ghizoni E, Denadai R, Raposo-Amaral CA, et al. Diagnosis of infant synostotic and nonsynostotic cranial deformities: a review for pediatricians. Rev Paul Pediatr. 2016;34(4):495–502. Article Summary in PubMed.
Sahrmann SA. The human movement system: our professional identity. Phys Ther. 2014;94:1034–1042. Article Summary in PubMed.
Cavalier A, Picot MC, Artiaga C, et al. Prevention of deformational plagiocephaly in neonates. Early Hum Dev. 2011;87(8):537–543. Article Summary in PubMed.
Fradette J, Gagnon I, Kennedy E, Snider L, Majnemer A. Clinical decision-making regarding intervention needs of infants with torticollis. Pediatr Phys Ther. 2011;23(3):249–256. Article Summary in PubMed.
Koren A, Reece SM, Kahn-D'angelo L, Medeiros D. Parental information and behaviors and provider practices related to tummy time and back to sleep. J Pediatric Health Care. 2010;24(4):222–230.
Hagan JF, Shaw JS, Duncan PM. Bright Futures: Guidelines for Health Supervision of Infants, Children and Adolescents. 3rd ed. Elk Grove Village, Illinois: The American Academy of Pediatrics; 2008.
Council on Children with Disabilities; Section on Developmental Behavioral Pediatrics; Bright Futures Steering Committee; Medical Home Initiatives for Children with Special Needs Project Advisory Committee. Identifying infants and young children with developmental disorders in the medical home: an algorithm for developmental surveillance and screening. Pediatrics. 2006;118(1):405–420. Article Summary in PubMed.
Siatkowski RM, Fortney AC, Nazir SA, et al. Visual field defects in deformational posterior plagiocephaly. J AAPOS. 2005;9(3):274–278. Article Summary in PubMed.
AAP Task Force on SIDS. The changing concept of sudden infant death syndrome: diagnostic coding shifts, controversies regarding the sleeping environment, and new variables to consider in reducing risk. Pediatrics. 2005;116(5):1245–1255. Article Summary in PubMed.
Chen MM, Chang HC, Hsieh CF, et al. Predictive model for congenital muscular torticollis: analysis of 1021 infants with sonography. Arch Phys Med Rehabil. 2005;86(11):2199–2203. Article Summary in PubMed.
Littlefield TR, Saba NM, Kelly KM. On the current incidence of deformational plagiocephaly: an estimation based on prospective registration at a single center. Semin Pediatr Neurol. 2004;11(4):301–304. Article Summary in PubMed.
Stellwagen LM, Hubbard E, Vaux K. Look for the "stuck baby" to identify congenital torticollis. Contemp Pediatr. 2004;21(5):55–65.
Biggs WS. Diagnosis and management of positional head deformity. Am Fam Physician. 2003;67(9):1953–1956. Article Summary in PubMed.
Littlefield TR, Kelly KM, Reiff JL, Pomatto JK. Car seats, infant carriers, and swings: their role in deformational plagiocephaly. J Prosthetics Orthotics. 2003;15(3):102–106.
Race/ethnicity, gender, socioeconomic status-research exploring their effects on child health: a subject review. Pediatrics. 2000;105(6):1349–1351. Article Summary in PubMed.
Littlefield TR, Kelly KM, Pomatto JK, Beals SP. Multiple-birth infants at higher risk for development of deformational plagiocephaly. Pediatrics. 1999;103:565-569. Article Summary in PubMed.
*PubMed is a free online resource developed by the National Center for Biotechnology Information. PubMed contains millions of citations to biomedical literature, including citations in the National Library of Medicine's MEDLINE database.
Expert Review:
May 29, 2022
Revised:
Jun 16, 2022
Content Type: Guide
Head-shape Flatness
PT, PhD, board-certified clinical specialist in pediatric physical therapy, on behalf of the Academy of Pediatric Physical Therapy
Taylor Huckfeldt
PT, DPT, on behalf of the Academy of Pediatric Physical Therapy
You Might Also Like...
Podcast
Plagiocephaly: Pediatric Treatment for Flat Head SyndromeAug 22, 2013
A physical therapist and orthotist discuss the treatment of plagiocephaly (or flat head syndrome) for babies.
Did You Know?
Almost Half of Babies Have Flat SpotsJul 13, 2013
Putting babies to sleep on their backs helps prevent sudden infant death syndrome, but it may have led to an increase in flat spots on babies' heads. If

