Physical Therapy Guide to Pelvic Pain
Pelvic pain is pain felt in the lower abdomen (stomach area), pelvis, or perineum (the area between the rectum and the scrotum or vagina). It has many possible causes. Pelvic pain affects up to 20% of people in the United States, including women and men. It is more common in women. Pelvic pain is called chronic when it lasts for more than six months.
Physical therapists help people with pelvic pain restore strength, flexibility, and function to the muscles and joints in the pelvic region. They help people get back to their everyday activities.
Physical therapists are movement experts. They improve quality of life through hands-on care, patient education, and prescribed movement. You can contact a physical therapist directly for an evaluation. To find a physical therapist in your area, visit Find a PT.
What Is Pelvic Pain?
The causes of pelvic pain can include:
- Pregnancy and childbirth, which affect pelvic muscles and cause changes to pelvic joints.
- Pelvic joint problems from causes other than pregnancy and childbirth.
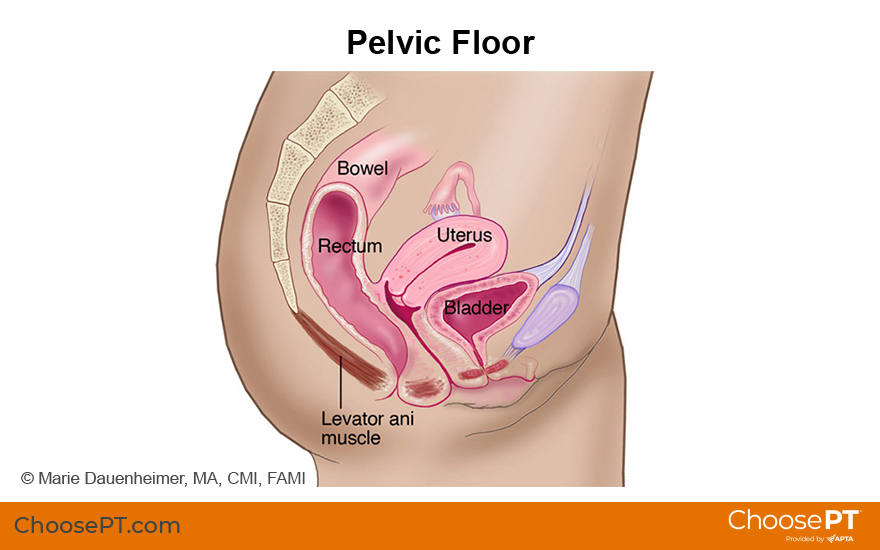
- Muscle weakness or imbalance within the muscles of the pelvic floor, trunk, or pelvis.
- Changes in the muscles that control the bowel and bladder.
- Tender areas in the muscles around the pelvis, abdomen (stomach area), low back, or groin areas.
- Pressure on one or more nerves in the pelvis.
- Weakness of the muscles around the pelvis, including the pelvic floor.
- Scar tissue after abdominal or pelvic surgery.
- Disease.
- A shift in the position of the pelvic organs, known as prolapse.
How Does It Feel?
The pain in your lower abdomen and pelvis may vary. Some people say it feels like an aching pain. Others describe it as a burning, sharp, or stabbing pain, or even like "pins and needles." You also may have:
- Pain in the hip or buttock.
- Pain in the tailbone or pubic bone.
- Pain in the joints of the pelvis.
- Tenderness in the muscles of the abdomen, low back, or buttock region.
- A sensation of heaviness in the pelvic region.
- A feeling that you are sitting on something hard, like a golf ball.
Signs and Symptoms
With pelvic pain, you may experience:
- Inability to sit for a long period.
- Reduced ability to move your hips or low back.
- Trouble walking, sleeping, or doing daily activities.
- Pain or numbness in the pelvic region with exercise or other activities, such as riding a bike or running.
- Pain during sexual activity.
- Urinary frequency, urgency, or incontinence, or pain during urination.
- Constipation, straining, or pain with bowel movements.
- Problems inserting tampons or with sexual penetration.
How Is It Diagnosed?
Your physical therapist will review your medical history and perform a physical exam to identify the causes of your pelvic pain. They will look for any joint issues, muscle tightness or weakness, or nerve involvement. The exam may include:
- Pelvic-girdle (the basin-shaped bony structure that connects the spine to the legs) screening.
- Soft-tissue assessment.
- Visual exam of the tissues.
- Sensation testing.
- Internal assessment of pelvic-floor muscles.
Your physical therapist also may refer you to a doctor to help in your plan of care.
How Can a Physical Therapist Help?
Based on their findings, your physical therapist will design a treatment program to meet your specific needs and goals. Your physical therapist may:
- Show you how to identify the appropriate muscles, such as the pelvic floor, deep abdominals, and diaphragm.
- Teach you how to use these muscles correctly. Your physical therapist can instruct you on the proper ways to do activities like:
- Exercise.
- Correcting your posture.
- Getting up from a chair.
- Squatting to pick up a child or an object from the floor.
- Work with you on exercises to stretch and strengthen the affected muscles. The goal is to help your muscles work together in the best way possible.
- Teach you the right pelvic-floor muscle exercises.
- Get you back to doing all of the activities you were able to do before your pelvic pain started.
Can This Injury or Condition Be Prevented?
Some risk factors affect general health and your core and pelvic muscle and joint strength. These include:
- Aging.
- Smoking and related coughing.
- Inactivity.
- Obesity.
- Childbirth.
Exercises may help improve muscle function and lower the risk of pelvic injury or pain. These can include:
- Core stability, pelvic-floor, and deep abdominal-wall exercises.
- Muscle flexibility training.
- Body-awareness exercises.
Your physical therapist will design the right treatment program for your specific condition. The main goal of physical therapy is to restore muscle strength and movement and help to relieve your pain.
What Kind of Physical Therapist Do I Need?
All physical therapists are prepared through education and experience to treat a variety of conditions or injuries. You may want to consider:
- A physical therapist who is experienced in treating people with pelvic health issues.
- A physical therapist who completed a residency or fellowship in women's health physical therapy. This physical therapist has advanced knowledge, experience, and skills that may apply to your condition.
- A physical therapist who is a board-certified specialist in women’s health physical therapy.
- A physical therapist who has earned a certificate from the CAPP-Pelvic program through the Academy of Pelvic Health Physical Therapy.
You can find physical therapists in your area with these credentials and clinical expertise on Find a PT, a tool built by the American Physical Therapy Association.
General tips when you're looking for a physical therapist (or any other health care provider):
- Get recommendations from family, friends, or other health care providers.
- When you contact a physical therapy clinic for an appointment, ask about the physical therapists' experience in helping people with pelvic pain.
- Be prepared to describe your symptoms in as much detail as possible during your first visit. Make a note of what makes your symptoms better or worse.
The American Physical Therapy Association believes that consumers should have access to information to help them make informed health care decisions and prepare them for their visit with a health care provider.
The following resources offer some of the best scientific evidence related to physical therapy treatment for pelvic pain. They report recent research and give an overview of the standards of practice both in the United States and internationally. They link to a PubMed* abstract that also may offer free access to the full text, or to other resources. You can read them or print out a copy to bring with you to your health care provider.
Trahan J, Leger E, Allen M, et al. The efficacy of manual therapy for treatment of dyspareunia in females: a systematic review. J Women's Health Phys Therap. 2019;43(1):28–35. Article Summary in PubMed .
Alappattu M, Hilton S, Bishop M. An international survey of commonly used interventions for management of pelvic pain. J Women's Health Phys Therap. 2019;43(2):82–88. Article Summary on PubMed.
Singh MK, Rivlin ME. Chronic pelvic pain in women. Medscape. Updated February 28, 2018.
Clinton SC, Newell A, Downey PA, Ferreira K. Pelvic girdle pain in the antepartum population: physical therapy clinical practice guidelines linked to the international classification of functioning, disability, and health from the Section on Women's Health and the Orthopaedic Section of the American Physical Therapy Association. J Women's Health Phys Therap. 2017;41(2):102–125. Free Article.
Ortiz DD. Chronic pelvic pain in women. Am Fam Physician. 2008;77(11):1535–1542. Article Summary in PubMed.
Fisher KA. Management of dyspareunia and associated levator ani muscle overactivity. Phys Ther. 2007;87(7):935–941. Article Summary in PubMed.
Borello-France DF, Handa VL, Brown MB, et al. Pelvic-floor muscle function in women with pelvic organ prolapse. Phys Ther. 2007;87(4):399–407. Article Summary in PubMed.
Stuge B, Holm I, Vollestad N. To treat or not to treat postpartum pelvic girdle pain with stabilizing exercises? Man Ther. 2006;11(4):337–343. Article Summary in PubMed.
Depledge J, McNair PJ, Keal-Smith C, Williams M. Management of symphysis pubis dysfunction during pregnancy using exercise and pelvic support belts. Phys Ther. 2005;85(12):1290–1300. Article Summary in PubMed.
* PubMed is a free online resource developed by the National Center for Biotechnology Information. PubMed contains millions of citations to biomedical literature, including citations in the National Library of Medicine’s MEDLINE database.
Expert Review:
May 25, 2021
Revised:
May 25, 2021
Content Type: Guide
Pelvic Pain
PT, DPT, board-certified clinical specialist in women's health physical therapy
an academy of the American Physical Therapy Association
Carina Siracusa
PT, DPT, board-certified clinical specialist in women’s health physical therapy and board-certified specialist in oncologic physical therapy
Jennifer Davia
PT, DPT, board-certified clinical specialist in women’s health physical therapy, on behalf of the Academy of Pelvic Health Physical Therapy
You Might Also Like...
Health Tips
From Pregnancy to Menopause: 4 Ways Physical Therapy Advances Women’s HealthApr 15, 2024
Physical therapy isn't only for rehabilitation from sports injuries or recovering after surgery? Physical therapists also play an important role in women's
Podcast
Overcoming Pelvic Floor Dysfunction and Pain in Women, Men, and RunnersSep 17, 2020
Amanda Olson sustained a severe injury that left her unable to sit for months. Now she is helping others overcome, anticipate, and prevent pelvic floor
Podcast
Treating Pelvic Pain in Transgender People: Keys to Respectful CareMay 16, 2019
Pelvic floor issues can be physically and emotionally painful — and embarrassing — for anyone. For a person who is transgender these issues can be


