Physical Therapy Guide to Jaw Fracture (Temporomandibular Joint Fracture)
Temporomandibular joint, or TMJ, fracture (jaw fracture) is the second most common fracture to the bones of the face. Only the bones of the nose are broken more frequently. The jawbone (mandible) or skull bone section of the jaw (temporal bone) may be broken near or through the TMJ. The injury normally occurs due to trauma to the face, such as a direct hit. The joint itself may be damaged, as well as the muscles that move the jaw. After the bone heals, it may be difficult to open or move the jaw. Physical therapists help people who have sustained TMJ fractures to relieve their pain and restore movement and function to the jaw.
Physical therapists are movement experts. They improve quality of life through hands-on care, patient education, and prescribed movement. You can contact a physical therapist directly for an evaluation. To find a physical therapist in your area, visit Find a PT.
What Is Temporomandibular Joint Fracture (Jaw Fracture)?
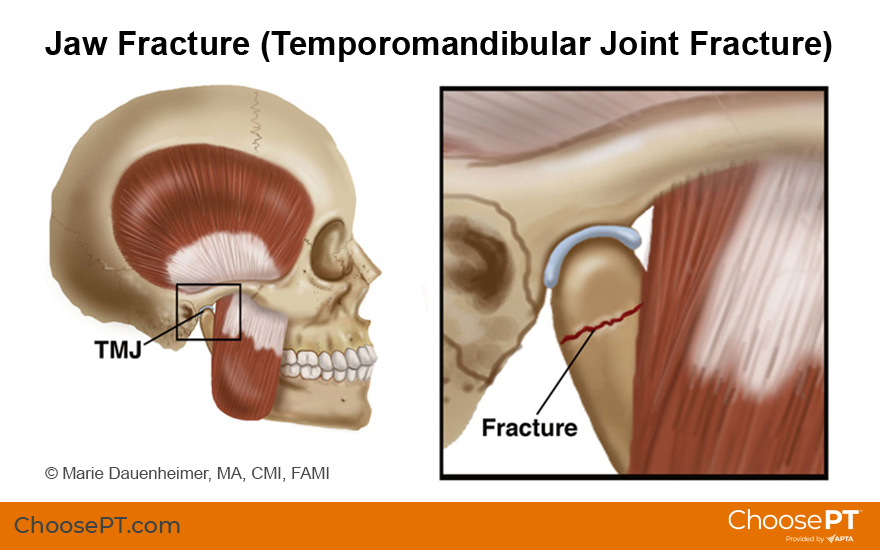
A temporomandibular joint fracture occurs when the mandible and/or temporal bone is broken near or through the TMJ, the joint connecting the jawbone to the skull. Like other bones in the body, the mandible, also known as the jawbone, and the temporal bone, the bone on the skull that forms the upper part of the jaw joint, can break when subjected to trauma. TMJ fractures occur due to direct trauma to the face. The jaw most often breaks along the condyles, which are rounded projections on the jawbone. Fracture also may occur with a dislocation of the joints.
Motor vehicle accidents, assaults, sports injuries, and falls are the most common causes of TMJ fractures. Men aged 20 to 29 years are most likely to sustain these injuries and are approximately three times more likely than women of the same age to do so.
Following a TMJ fracture, especially if the inside surface of the mouth is torn, there also is a risk of infection, which can lead to osteomyelitis of the jaw. Blows to the head severe enough to cause a TMJ fracture can also cause a concussion.
How Does It Feel?
Following a TMJ fracture, you may experience:
- Jaw pain.
- Swelling and possible bruising in the area.
- Jaw fatigue.
- Difficulty opening your mouth to eat or talk.
- Ringing in your ears.
- Dizziness.
- Headache.
- Loose or broken teeth.
- Popping sounds in your jaw.
- Neck pain.
- A change in the way the teeth fit together.
- A locking jaw.
- A bump you can feel with your fingers on the jaw bone or joint.
How Is It Diagnosed?
In cases of facial trauma and pain, a diagnosis is made by an emergency medicine physician at a hospital or other emergency clinic. X-rays or a CT scan will be ordered to determine the existence and severity of a fracture. If the jaw is dislocated, the physician will return it to its normal position.
- A less severe fracture is diagnosed when the bone is still in place but has a small fracture line where the bone has broken.
- A more severe fracture can involve a larger fracture line, partially displaced sections of bone, or a dislocation.
- An extreme fracture involves displaced segments of bone or fragmented bone with a significant alteration of bone structure.
There are several treatments to help a TMJ fracture safely heal.
- If the fracture is less severe, your physician will recommend resting the jaw by:
- Eating soft foods or going on a liquid diet.
- Limiting jaw use such as speaking or brushing your teeth.
- If the fracture is severe, your physician may consider a form of splint therapy to hold the jaw steady and rest it in a proper position for healing.
- If the fracture is extreme, surgery may be required, or the jaw may be set and wired closed to prevent any movement and ensure complete healing.
All of these treatments allow the jaw to heal but often result in TMJ stiffness. The muscles used to move the jaw also may become tight and weak. You may not be able to eat, drink, or open your mouth as you normally would. Your physical therapist will work with you to help restore your jaw's normal movement, function, and muscular strength.
How Can a Physical Therapist Help?

Once you have completed a course of rest or splinting, your physical therapist can help restore the natural movement of your jaw and decrease your pain. During your first visit, your physical therapist may:
- Review your medical history and discuss any previous surgery, fractures, or other injuries to your head, neck, or jaw.
- Evaluate the quality and quantity of movement in your jaw and neck.
- Assess your posture and observe how your neck moves.
- Examine the TMJ to find out how well it can open and whether there are any abnormalities in jaw motion following the fracture.
Following the examination, your physical therapist will select the appropriate treatments to improve your jaw movement and relieve your pain.
Improving Your Jaw Movement
Stretching and motion exercises. Your physical therapist may prescribe stretches and range-of-motion exercises for the jaw. The instruction will include guidelines for frequency and intensity of movement to ensure your safe performance of all your exercises.
Manual therapy. Your physical therapist may also apply skilled hands-on techniques (manual therapy) to gently increase your jaw movement and relieve your pain.
"Low-load" exercises. Your physical therapist may teach you special "low-load" strengthening exercises that don't exert a lot of pressure on your TMJ but can help strengthen the muscles of the jaw and restore a more natural, pain-free motion. Your physical therapist also will teach you exercises that help you increase the opening of your jaw and improve the way it works.
Relieving Your Pain
If your pain is severe, your physical therapist may apply physical modalities, such as electrical stimulation or deep heat, to reduce pain and improve motion.
Can This Injury or Condition Be Prevented?
As TMJ fractures result from trauma to the face, avoiding situations that lead to violent behavior or accidents is key to prevention. Wearing proper helmets and mouth guards will help you avoid sports-related TMJ fractures. Safe driving practices reduce motor-vehicle accidents, but in the event of an accident, wearing your seat belt will reduce traumatic forces to the face and head. Preventing falls with proper footwear, keeping walking paths clear, and other safety practices also help reduce risk. Your physical therapist can help assess your home and work environments and your daily activities to lessen your risk of injury.
What Kind of Physical Therapist Do I Need?
All physical therapists are prepared through education and experience to treat patients who have bone fractures. You may want to consider:
- A physical therapist who is experienced in treating people with orthopedic or musculoskeletal problems. Some physical therapists have a practice with a craniofacial focus, meaning that they focus on movement disorders related to the skull and facial structures.
- A physical therapist who is a board-certified clinical specialist or who completed a residency or fellowship in orthopaedics physical therapy. This therapist has advanced knowledge, experience, and skills that may apply to your condition.
You can find physical therapists who have these and other credentials by using Find a PT, the online tool built by the American Physical Therapy Association to help you search for physical therapists with specific clinical expertise in your geographic area.
General tips when you're looking for a physical therapist (or any other health care provider):
- Get recommendations from family and friends or from other health care providers.
- When you contact a physical therapy clinic for an appointment, ask about the physical therapists' experience in helping people with TMJ fracture.
- Be prepared to describe your symptoms in as much detail as possible, and say what makes your symptoms worse.
The American Physical Therapy Association believes that consumers should have access to information that could help them make health care decisions and also prepare them for a visit with their health care provider.
The following articles provide some of the best scientific evidence related to physical therapy treatment of jaw fracture. The articles report recent research and give an overview of the standards of practice both in the United States and internationally. The article titles are linked either to a PubMed* abstract of the article or to free full text, so that you can read it or print out a copy to bring with you to your health care provider.
Adik K, Lamb P, Moran M, et al. Trends in mandibular fractures in the USA: a 20-year retrospective analysis. Dent Traumatol. 2023;39(5):425–436. Article Summary on PubMed
Shaffer SM, Naze GS. Evaluation and management of temporomandibular disorders. Part 1: an orthopedic physical therapy update on examination and clinical reasoning. J Man Manip Ther. 2023;31(3):133–142. Article Summary on PubMed
Shaffer SM, Naze GS. Evaluation and management of temporomandibular disorders. Part 2: an orthopaedic physical therapy update on examination and clinical reasoning. J Man Manip Ther. 2023;31(3):143–152. Article Summary on PubMed
Wadhokar OC, Patil DS. Current trends in the management of temporomandibular joint dysfunction: a review. Cureus. 2022;14(9):e29314. Article Summary on PubMed
Butts R, Dunning J, Pavkovich R, et al. Conservative management of temporomandibular dysfunction: a literature review with implications for clinical practice guidelines (Narrative review part 2). J Bodyw Mov Ther. 2017;21(3):541–548. Article Summary on PubMed
*PubMed is a free online resource developed by the National Center for Biotechnology Information. PubMed contains millions of citations to biomedical literature, including citations in the National Library of Medicine’s MEDLINE database.
Expert Review:
Jul 1, 2024
Revised:
Sep 27, 2024
Content Type: Guide
Jaw Fracture
PT, DPT, MTC, FAAOMPT
Laura Thornton
PT, MPT, Board-Certified Clinical Specialist in Orthopaedic Physical Therapy and Fellow of the American Academy of Orthopaedic Manual Physical Therapy, on behalf of the Academy of Orthopaedic Physical Therapy.