Physical Therapy Guide to Groin Strain
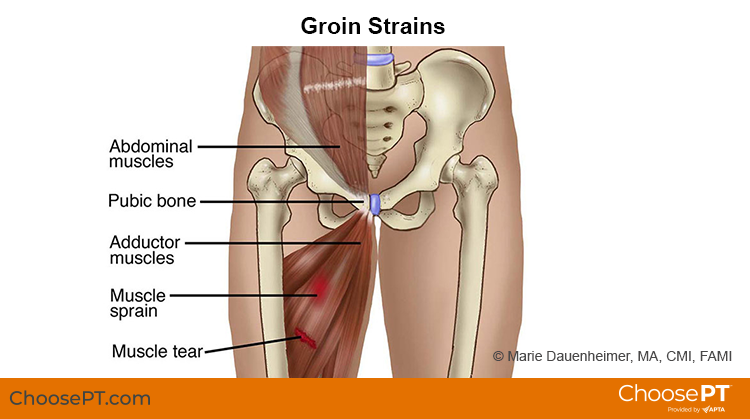
A groin strain is an injury to the area of the body where the abdomen meets the leg and the inner thigh muscles (adductors) attach to the pubic bone. Typically, groin strains occur in the muscles of the upper inner thigh near the pubic bone or in the front of the hip. This injury is more common in athletes and men, but certain activities can increase the risk of groin strain for anyone.
Groin strains can occur during sprinting or with any type of activity requiring forceful movement of the leg. These can include jumping, kicking the leg up, or changing directions while running. Groin strains account for 10% of all hockey injuries and 5% of all soccer injuries. Physical therapists treat groin strains by reducing pain and helping patients improve muscle strength and leg motion. Physical therapy can also help to reduce recovery time.
Physical therapists are movement experts. They improve quality of life through hands-on care, patient education, and prescribed movement. You can contact a physical therapist directly for an evaluation. To find a physical therapist in your area, visit Find a PT.
What Is a Groin Strain?
A groin strain is an overstretching or tearing injury to the muscles of the inner thigh or front of the hip. Groin strains make certain activities hard to do and painful. These can include walking, lifting the knee, or moving the leg away from or toward the body. Groin strains can occur from overuse of the muscles. They also can result from a sudden contraction (such as tightening) of the muscles.
Injury occurs when the muscles are either too forcefully contracted or too forcefully overstretched. There are several grades of groin strains based on the amount of muscle damage that occurs. They are:
- Grade 1. Mild or partial stretch, or a tear of a few muscle fibers. The muscle is tender and painful but maintains its normal strength. Use of the leg is not impaired, and walking is normal.
- Grade 2. Moderate stretch or tearing of a greater percentage of the muscle fibers. There is more tenderness and pain, noticeable loss of strength, and sometimes bruising. Use of the leg is noticeably impaired, and limping when walking is common.
- Grade 3. Severe tear of the muscle fibers, sometimes a complete muscle tear. A "popping" sound may be heard or felt when the injury occurs. Bruising is apparent. A "dent" in the muscle may be seen under the skin at the site of the tear. Use of the leg is very difficult, and putting weight on the leg is very painful.
Groin strains most often occur in athletic activities such as football, soccer, and dance. They also can occur during everyday activities, such as lifting heavy items or slipping while walking. With a groin strain or tear, muscle fibers and other cells are disrupted. Bleeding can occur, which causes bruising. Within a few minutes to a few hours after the injury, swelling can occur. This can cause the injured area to expand and feel tight and stiff.
How Does It Feel?
A groin strain causes sharp pain or spasms in the groin area or lower abdominal region. The pain can quickly resolve, or it can last. It can become a throbbing pain at rest with sharp stabs of pain when you try to move your leg or walk.
A lower-grade strain can be relatively pain free with everyday activities and walking. However, it can become aggravated with quick movements of the legs. These can include cutting, kicking, performing sit-ups, or sprinting/running.
Higher-grade strains can cause the muscles to feel tight or weak. Simple movements that involve lifting the leg or knee or bringing the knees together can provoke pain. This can even cause the groin muscles to spasm. With a Grade 3 injury, using the leg at all can be extremely painful.
Risk Factors
There are several risks factors for groin strains. They include:
- Male sex.
- Previous groin injury.
- Groin pain in previous athletic season.
- Hip weakness (both hip abductors and hip adductors).
Signs and Symptoms
With a groin strain, you may experience one or more of the following symptoms in the groin area or lower abdomen:
- Pain, a deep ache, and/or spasms.
- Swelling.
- Bruising.
- Tightness.
Additional symptoms that you may experience include:
- Weakness in the leg when trying to walk, climb stairs, or move the leg.
- Limping when walking.
- Difficulty performing daily activities that require standing and walking.
How Is It Diagnosed?
If you see your physical therapist first, they will conduct a thorough evaluation that includes taking your health history. The first goal of your physical therapist is to rule out any other serious conditions that may be causing your symptoms. Groin pain can be present with other diagnoses involving your hip, pelvis, or lower back. Your physical therapist may ask specific questions or use tests to tell if other areas of your body are causing your pain.
Your physical therapist may ask you:
- What were you doing when you first felt pain?
- Where did you feel the pain?
- Did you hear a “pop” when it occurred?
- Did you receive a direct hit to your leg or groin area?
- Did you notice any swelling in the first two to three hours after the injury?
- Do you feel pain when lifting your leg, walking, moving the leg away from you, or drawing your knees together?
Your physical therapist will perform an examination to diagnose your condition. It may include:
- Gently moving your leg away from your body.
- Asking you to resist against their hand as they try to gently push your leg outward (muscle strength test).
- Gently feeling parts of the muscle to find the specific location of the injury (palpation).
To provide a final diagnosis, your physical therapist may collaborate with an orthopedist or other health care provider. The orthopedist may order further tests — such as an X-ray or MRI. These can help confirm their diagnosis and rule out other issues. Such tests, however, are not commonly required for groin strain.
How Can a Physical Therapist Help?
Your physical therapist will design a treatment program for your specific needs to speed your recovery. The program will include exercises and treatments you can do at home to help you return to your normal lifestyle and activities. Your physical therapist will personalize a treatment plan for you based on your unique condition and goals.
During the First 24 to 48 Hours After Injury
Your physical therapist may advise you to:
- Rest the area. This may include avoiding walking or any activity that causes pain. They may recommend crutches to reduce further strain on the muscles when walking.
- Apply ice packs to the area.
- Compress the area with an elastic bandage wrap.
- Consult with another health care provider for further services. These may include medication or diagnostic tests.
As you continue with recovery from your groin strain, your individualized plan may include treatments to:
Reduce pain. Your physical therapist may use different treatments for pain. These may include ice, heat, ultrasound, electrical stimulation, taping, exercises, and hands-on therapy such as massage. These treatments can lessen the need for pain medication, including opioids.
Improve motion. Your physical therapist will choose specific activities and treatments to help restore normal movement in the leg and hip. These might begin with "passive" motions that they perform for you to gently move your leg and hip joint. They will help you progress to doing active exercises and stretches that you perform yourself.
Improve strength. Certain exercises will benefit healing at each stage of recovery. Your physical therapist will teach you the appropriate exercises to restore your strength and agility. These may include using cuff weights, elastic bands, weight-lifting equipment, and cardio-exercise equipment, such as treadmills or stationary bicycles.
Speed recovery time. Your physical therapist is trained and experienced in choosing the right treatments and exercises to help you heal. They can help you return to your normal lifestyle and reach your goals faster than you are likely to do on your own.
Promote a safe return to activities. Your physical therapist will work with you to decide on your recovery goals, including your return to work or sport. They will design your treatment program to help you reach those goals in the safest, fastest, and most effective way possible. Your physical therapist can teach you work retraining activities. They also may teach you sport-specific techniques and drills to help you achieve any sport-specific goals.
Prevent future reinjury. Your physical therapist can recommend a home exercise program to strengthen and stretch the muscles around your hip, upper leg, and abdomen. Doing these prescribed exercises can help prevent future reinjury of your groin. These may include strength and flexibility exercises for the leg, hip, and core muscles.
If Surgery Is Necessary
Surgery is rarely needed for a groin strain. If a groin muscle fully tears and requires surgical repair, your physical therapist will help you minimize pain, restore motion and strength, and return to normal activities safely and as soon as possible after surgery.
Can This Injury or Condition Be Prevented?
The following recommendations can help you prevent a groin strain:
- Increase the intensity of activity or sport gradually, not suddenly. Avoid pushing yourself too hard, too fast, too soon.
- Always warm up before starting a sport or heavy physical activity.
- Follow a consistent strength and flexibility exercise program to maintain good physical conditioning, even in a sport's off-season.
- Strengthen the muscles of the inner thigh, groin, and buttocks.
- Wear shoes that are in good condition and fit well.
- Use correct lifting techniques.
Your physical therapist can help you learn more about any of these recommendations and offer specific training to help you achieve them.
What Kind of Physical Therapist Do I Need?
All physical therapists are prepared through education and experience to treat groin strains. However, you may want to consider:
- A physical therapist who is experienced in treating people with groin strains.
- A physical therapist who focuses their practice in orthopedics or sports rehabilitation.
- A physical therapist who is a board-certified clinical specialist or who completed a residency or fellowship in sports physical therapy. This physical therapist has advanced knowledge, experience, and skills that may apply to your condition.
You can search for physical therapists in your area who have these and other credentials by using Find a PT, the online tool built by the American Physical Therapy Association.
General tips when you're looking for a physical therapist (or any other health care provider):
- Get recommendations from family, friends, or other health care providers.
- When you contact a physical therapy clinic for an appointment, ask about the physical therapists' experience in helping people who have groin strains.
- Be prepared to describe your symptoms in as much detail as possible, and describe what makes your symptoms worse.
The American Physical Therapy Association believes that consumers should have access to information that could help them make health care decisions and also prepare them for a visit with their health care provider.
The following articles provide some of the best scientific evidence related to physical therapy treatment of groin strain. The articles report recent research and give an overview of the standards of practice both in the United States and internationally. The article titles are linked either to a PubMed* abstract of the article or to free full text, so that you can read it or print out a copy to bring with you to your health care provider.
Alsirhani AA, Muaidi QI, Nuhmani S, et al. The effectiveness of the Copenhagen adduction exercise on improving eccentric hip adduction strength among soccer players with groin injury: a randomized controlled trial. Phys Sportsmed. 2024;52(5):497–506. Article Summary in PubMed .
Thorborg K. Current clinical concepts: exercise and load management of adductor strains, adductor ruptures, and long-standing adductor-related groin pain. J Athl Train. 2023;58(7-8):589–601. Article Summary in PubMed .
Rodriguez R. Measuring the hip adductor to abductor strength ratio in ice hockey and soccer players: a critically appraised topic. J Sport Rehabil. 2020;29(1):116–121. Article Summary in PubMed .
Schöberl M, Prantl L, Loose O, et al. Non-surgical treatment of pubic overload and groin pain in amateur football players: a prospective double-blinded randomised controlled study. Knee Surg Sports Traumatol Arthrosc. 2017;25(6):1958–1966. Article Summary in PubMed .
*PubMed is a free online resource developed by the National Center for Biotechnology Information. PubMed contains millions of citations to biomedical literature, including citations in the National Library of Medicine's MEDLINE database.
Expert Review:
Dec 3, 2024
Revised:
Jan 31, 2025
Content Type: Guide
Groin Strain
PT, DPT
Derek Sople
PT, DPT, board-certified clinical specialist in orthopaedic physical therapy
James E. Zachazewski
PT, DPT, board-certified clinical specialist in sports physical therapy, on behalf of the American Academy of Sports Physical Therapy