Physical Therapy Guide to Collarbone Fracture (Clavicle Fracture)
The collarbone, or clavicle, connects the arm to the body. It helps stabilize the shoulder and arm as they move. A collarbone fracture is a common shoulder injury. It makes up 4% of all fracture types and 35% of all shoulder injuries. The injury is most often caused by trauma, such as a direct blow to the shoulder or a fall. It occurs most often in young men under age 20, often as a result of a sports injury. Collarbone fractures also often result from a fall in older adults. Men typically fracture their collarbones in their younger years. Collarbone fractures in women are more common with older age.
Most collarbone fractures are treated without surgery. However, more severe fractures may require surgery. Physical therapists treat collarbone fractures before and after surgery. They provide pain management, guided exercise, and functional training during the healing process.
Physical therapists are movement experts. They improve quality of life through hands-on care, patient education, and prescribed movement. You can contact a physical therapist directly for an evaluation. To find a physical therapist in your area, visit Find a PT.
What Is a Clavicle Fracture?
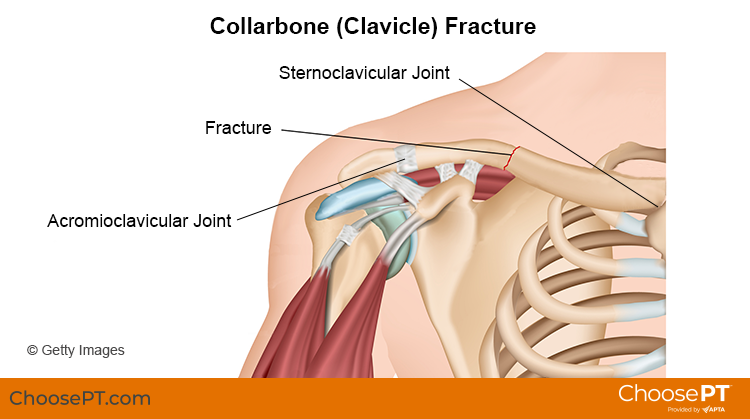
The collarbone (clavicle) is located on the front of the chest and shoulder. It connects the arm to the body by two joints:
- Sternoclavicular joint. This is where the clavicle connects to the sternum (breast bone).
- Acromioclavicular joint. This is where the clavicle connects to the scapula (shoulder blade).
The collarbone helps stabilize the shoulder during movement. It also helps protect nerves and blood vessels that extend from the neck and connect into the upper extremity.
Clavicle fractures are classified according to the place where the bone is broken. They are:
- Midshaft (middle of the bone). This type usually occurs in younger people and makes up 75% to 80% of all collarbone fractures.
- Lateral-end (near the acromioclavicular joint). About 15% to 25% of all collarbone fractures are lateral-end fractures.
- Medial-end (near the sternoclavicular joint). This type is rare, making up just 5% of all collarbone fractures.
Health care providers also describe fractures as:
- Nondisplaced. The pieces of the fractured bone remain lined up.
- Displaced. The two parts of the fractured bone do not line up.
- Comminuted. Splinters or small pieces of bone are found at the fracture site.
- Compound. When the bone pierces (goes through) the skin.
How Does It Feel?
If you break your collarbone, you will experience pain in the immediate area of the break. Other signs and symptoms may include:
- Pain in the general area of the collarbone. Arm pain or discomfort (in more severe cases).
- Bruising, which may spread to the shoulder and arm.
- Swelling that occurs at the injury site and in the arm.
- Lack of ability to lift the arm. Most people will hold their arm close to their body or support their arm with the other hand.
- A grinding or shifting feeling of the bone when moving the arm.
- A bump at the injured area. The skin may lift in the location of the fracture, like a tent.
How Is It Diagnosed?
Your physical therapist will perform a full evaluation whether or not you have surgery. The goals of the exam are to assess the degree of your condition or injury. It also helps to determine the cause and any factors that may have contributed to it. Collarbone fractures often result from a single injury.
Your physical therapist will interview you about your health history, injury, condition, and activities.
Forms you fill out before your first session help your physical therapist gather needed information. The interview will become more specific to the symptoms of a collarbone fracture. Your physical therapist may ask you questions such as:
- How did your injury occur?
- How have you taken care of the condition, such as seeing other health care providers? Have you had imaging or other tests and received their results?
- What are your current symptoms, and how have they changed your typical day and activities?
- Do you have pain, and if so, what is the location and intensity of your pain? Does pain vary during the day?
- Do you have trouble doing any activities? What activities are you unable to do since your injury? What activities make your symptoms worse? How do you reduce your symptoms?
This information allows the physical therapist to better understand what you are experiencing. It also helps determine the course of your physical exam.
The physical exam will vary depending on your interview. Most often it will begin with observing the movements discussed in the interview or any positions that cause you pain. The exam will include the area of your symptoms. It also may include other areas of the body that may have changed because of the injury.
Your physical therapist may watch you raise and lower your shoulder and arm. They will assess the mobility and strength of your shoulder, and other areas as needed. This will help them find what areas need treatment to improve your condition. Your physical therapist will gently, but skillfully, press around your upper arm and shoulder to find exactly where it is most painful.
Your physical therapist will discuss their findings with you. They will work with you to develop a program specific to you to help you recover.
How Can a Physical Therapist Help?
Most collarbone fractures are treated without surgery. The involved arm will be secured in a sling or a figure-eight brace for support and comfort. Physical therapy usually begins early to help reduce pain and swelling.
Healing times vary from person to person due to differences in age, health, and the extent of the injury. Many patients return to light daily activity after about six weeks. Generally, people can return to more strenuous job duties after nine to 12 weeks.
Your physical therapy treatment program may include some or all of the following:
Patient education. Your physical therapist will teach you about your injury. They will work with you to find any external factors that may have contributed to your injury. Your physical therapist also will recommend ways to change these factors and modify your daily activities.
Pain management. Your physical therapist will design a program to address your pain. This may include treatments such as applying ice to the affected area. They also may recommend changing some activities that cause pain. Physical therapists are experts in helping people manage pain. They can help you reduce or avoid the need for medicines, including opioids.
Range-of-motion exercises. With a collarbone injury, your movement may be limited. This can cause increased stress on your neck or other areas of the arm. In addition, a restriction in the area may force other parts of your neck or arm to work harder. Your physical therapist may teach you self-stretching methods. These will help to decrease tension and restore normal motion of the joints in your upper arm and shoulder.
Manual therapy. Your physical therapist may use hands-on (manual) therapy to gently move your muscles and joints to help improve motion. They also may provide hands-on therapy to guide your joints into a less stressful movement pattern. Your physical therapist also may use their hands to apply resistance while you do exercises to improve strength in the affected muscles.
Muscle strengthening. Muscle weaknesses or imbalances can contribute to ongoing symptoms. Your physical therapist will design a safe strengthening program for you. It likely will include your core (midsection) and the upper arm and shoulder area. Your program may include doing exercises in different positions, including standing or lying on your back. They may have you use elastic bands, tubing, or other equipment to provide resistance. Your physical therapist will choose exercises that are right for you based on your restrictions, pain level, and fitness.
Functional training. Once your pain, strength, and motion improve, you will need to safely transition back to more demanding activities. To minimize the stress on your collarbone and shoulder, it is important to learn safe, controlled movements. Your physical therapist will create a series of activities to help you learn how to use and move your body correctly and safely.
Braces and other assistive devices. Your physical therapist will work with you and other health care providers to determine if bracing will help you. Braces may be used for a short time, to rest the area.
Treatment After Surgery
Physical therapy after surgery is similar to that provided for people who do not need surgery. However after surgery, your program will progress by following a strict schedule set by your surgeon. It is typical for physical therapy to begin immediately following the operation. Eight to 12 weeks of physical therapy is common after surgery.
During the first week after surgery, your physical therapist will help you control pain and swelling. They may begin some gentle motion exercises. You will wear a sling or brace for support and comfort.
Over the next few weeks, your physical therapist will help you gradually increase your exercise program.
After about four weeks. If X-rays show good collarbone position and stability, your physical therapist will guide you to achieve full shoulder range of motion.
At six to eight weeks. If X-rays show enough healing, treatment will progress to include strengthening and resistance exercises.
These time frames will vary based on your age, health, the extent of your injury, and any surgery you had.
Can This Injury or Condition Be Prevented?
Not all collarbone fractures can be prevented. However, you can reduce your risk of injury by wearing appropriate protective gear when playing sports, such as properly fitted shoulder pads for football. Physical therapists work with athletes to improve their strength and movement. They help to ensure that you can safely perform at your best.
You also can reduce your risk by avoiding falls. To reduce your fall risk, it is important to keep strength and fitness throughout your life. It also is important to remove any tripping hazards (such as throw rugs, slippery floors).
What Kind of Physical Therapist Do I Need?
All physical therapists are prepared through education and experience to treat collarbone fractures. However, you may want to consider:
- A physical therapist who has experience treating sports or orthopedic injuries or pediatric conditions. Some physical therapists have a practice with a focus on sports medicine or orthopedics.
- A physical therapist who is a board-certified clinical specialist, or who completed a residency or fellowship in orthopedics or sports physical therapy. This physical therapist has advanced knowledge, experience, and skills that may apply to your condition.
You can find physical therapists in your area with these credentials and clinical expertise on Find a PT, a tool built by the American Physical Therapy Association.
General tips when you're looking for a physical therapist (or any other health care provider):
- Get recommendations from family, friends, or other health care providers.
- When you contact a physical therapy clinic for an appointment, ask about the physical therapists' experience in helping people who have fractured a clavicle/collarbone.
- Be prepared to describe your symptoms in as much detail as possible during your first visit. Make a note of what makes your symptoms better or worse.
The American Physical Therapy Association believes that consumers should have access to information to help them make informed health care decisions and prepare them for their visit with a health care provider.
The following resources offer some of the best scientific evidence related to physical therapy treatment for collarbone fractures. They report recent research and give an overview of the standards of practice both in the United States and internationally. They link to a PubMed* abstract that also may offer free access to the full text, or to other resources. You can read them or print out a copy to bring with you to your health care provider.
Catapano M, Hoppe D, Henry P, Nam D, Robinson LR, Wasserstein D. Healing, pain and function after midshaft clavicular fractures: a systematic review of treatment with immobilization and rehabilitation. PM R. 2019;11(4):401–408. Article Summary in PubMed.
Lenza M, Buchbinder R, Johnston RV, Ferrari BA, Faloppa F. Surgical versus conservative interventions for treating fractures of the middle third of the clavicle. Cochrane Database Syst Rev. 2019;1(1):CD009363. Article Summary in PubMed.
OrthoInfo. Clavicle fracture (broken collar bone). American Academy of Orthopaedic Surgeons’ website. Reviewed December 2016. Accessed July 12, 2021.
Donnelly TD, Macfarlane RJ, Nagy MT, Ralte P, Waseem M. Fractures of the clavicle: an overview. Open Orthop J. 2013;7: 329–333. Article Summary in PubMed.
*PubMed is a free online resource developed by the National Center for Biotechnology Information. PubMed contains millions of citations to biomedical literature, including citations in the National Library of Medicine’s MEDLINE database.
Expert Review:
Apr 28, 2021
Revised:
Apr 28, 2021
Content Type: Guide
Collarbone Fracture
PT, board-certified clinical specialist in orthopaedic physical therapy
Lisa Noceti-DeWit
PT, DPT, board-certified clinical specialist in orthopaedic and sports physical therapy
Stephen F. Reischl
PT, DPT, board-certified clinical specialist in orthopaedic physical therapy, on behalf of the Academy of Orthopaedic Physical Therapy